 |
 |


- Search
| Int Neurourol J > Volume 25(4); 2021 > Article |
|
ABSTRACT
Purpose
Transcutaneous tibial nerve stimulation (TTNS) has proven to be a valuable treatment option for various lower urinary tract conditions, such as overactive bladder syndrome and neurogenic detrusor overactivity. The aim of this study was to investigate acute changes in urodynamic parameters due to bilateral TTNS.
Methods
Fifty-one patients (18ŌĆō87 years; 61% female) with various lower urinary tract symptoms were enrolled in this study. They were single-blinded and randomly assigned to receive simultaneous bilateral TTNS either during their first urodynamic examination, followed by a second round using a placebo stimulation technique, or vice versa.
Results
For subjects without signs of anatomical pathologies, the filling volume at the first desire to void (FDV) increased significantly by 54 mL (interquartile range [IQR], 26ŌĆō81 mL; P<0.01) under the influence of TTNS compared to placebo. The maximum cystometric capacity increased by 41 mL (IQR, 10ŌĆō65 mL; P=0.02). The median micturition volume of patients with pathological postvoid residual volumes (>100 mL) increased by 76 mL compared to patients without urinary retention (IQR, 6ŌĆō166 mL; P=0.03).
Conclusions
Compared to placebo, simultaneous bilateral TTNS showed significant improvements in bladder functioning, such as delayed FDV, increased maximum cystometric capacity, and reduced urinary retention. Patients with signs of anatomical pathologies did not seem to benefit from TTNS. Further studies need to be conducted to compare the effectiveness of bilateral versus unilateral TTNS.
Over the past decades, an alternative, conservative, and cost-effective treatment option for lower urinary tract symptoms (LUTS) called tibial nerve stimulation (TNS) has been established. It is most commonly used for patients with overactive bladder syndrome (OABS) who do not respond to behavioral or anticholinergic treatment [1]. However, it has also proven to be a useful therapy for neurogenic detrusor overactivity (DOA), chronic pelvic pain syndrome, and fecal incontinence [2,3].
This method of neuromodulation was first proposed and successfully tested by McGuire et al. in 1983 [4]. It was originally developed as an electroacupuncture technique to stimulate the tibial nerve near the inner ankle. The treatment protocol usually consists of weekly 30-minute sessions for a period of 12 weeks, followed by an individualized maintenance scheme [5]. As Ram├Łrez-Garc├Ła et al. [6] have recently shown, using 2 surface skin electrodes for transcutaneous tibial nerve stimulation (TTNS) are safer and easier to apply than the needle-based percutaneous approach while demonstrating noninferiority in its clinical efficacy. Interestingly, TNS shows some similarities to Asian acupuncture techniques, but it is more commonly perceived as a peripheral, minimally invasive type of sacral neuromodulation (SNM) [7]. The reason for this perception is that TNS and SNM both share the same postulated mechanism of action: Even though it is yet to be fully understood, it seems that stimulating the S3 nerve root (either directly via SNM or mediated by the posterior tibial nerve, which contains L4ŌĆōS3 fibers) at a relatively low amplitude modulates the neural activity of several pathways involved in bladder control. Since the S3 root consists of afferent and efferent fibers, it is hypothesized that neuromodulation mutes sensory input and inhibits motoric reflex circuits (e.g., in the pontine micturition center) [7].
Various clinical findings support this hypothesis. A study of 70 patients with LUTS due to multiple sclerosis showed an average reduction of daytime voids by 2ŌĆō6 times, of nocturia by 2ŌĆō3 times, and 2.7 fewer incontinence episodes per week. Concomitantly, the average voided volume increased by 43ŌĆō89 mL and the postvoid residual volume decreased by 16ŌĆō55 mL [8]. A systematic review of TTNS for the treatment of OABS reported significant symptom improvements in 48%ŌĆō93% of all participants and cessation of urinary incontinence in 25%ŌĆō45% of all cases [9]. Amarenco et al. [10] examined urodynamic changes during acute TNS in 44 patients with DOA and found an increase of the mean maximum bladder capacity from 221 to 277 mL ( ┬▒130 and ┬▒118 mL, respectively; P <0.0001). Regular TNS sessions can lead to the maintenance of health benefits for at least 24 months [1].
Since little evidence exists regarding the acute effects of TTNS, the aim of this study was to evaluate immediate changes in urodynamics compared to placebo treatment. Even though bilateral TTNS has already effectively been used for proctologic conditions, this isŌĆöto the authorsŌĆÖ knowledgeŌĆöone of the first studies to examine the impact of simultaneous bilateral TTNS on urologic disorders [2,11].
Fifty-one adult patients with various LUTS were enrolled from July to September 2016 (Fig. 1). The inclusion criteria were urgency, urge urinary incontinence, and retention. Sixteen potential candidates were not enrolled since they met the exclusion criteria, which were nonage, pregnancy, epilepsy, previous electrostimulation, electronic or metallic implants, and any condition affecting stimulation site (e.g., skin lesion). Only patients who required a urodynamic examination according to the European Association of Urology guidelines regarding urinary incontinence, neurogenic bladder, and male LUTS were included in this trial after obtaining their written informed consent. To assess their individual symptoms, all the subjects were asked to fill in several validated questionnaires, translated into German, including the Urinary Incontinence Quality of Life Questionnaire (I-QoL), the International Consultation on Incontinence Modular Questionnaire Short Form (ICIQ-SF 2004) and the Overactive Bladder Symptom Score (OABSS) [12-14]. ParticipantsŌĆÖ medical history and prevalent symptoms were recorded, and a thorough physical examination was performed to identify potential anatomical pathologies such as cystocele or prostate enlargement. Furthermore, participants had to keep a bladder diary for 3 days.
Urodynamic testing, guided by good urodynamic practices, consisted of 2 urodynamic cycles in close succession [15]. Every urodynamic cycle involved a bladder filling phase (cystometry) followed by a bladder voiding phase (pressure-flow study). Bladder filling was done with 0.9% sodium chloride solution at 37┬░C, and the mean filling rate (in mL/min) was about a quarter of the respective body weight (in kg). An Ellipse device and the AUDACT software (both by ANDROMEDA Medizinische Systeme GmbH, Taufkirchen, Germany) were used for urodynamic testing. Several urodynamic parameters were assessed, such as bladder volume at first desire to void (FDV) (reference range 200ŌĆō330 mL), maximum cystometric capacity (350ŌĆō550 mL), bladder compliance (above 30 mL/cm H2O), voided volume (350ŌĆō550 mL), and detrusor pressure at maximum urine flow rate (18ŌĆō30 cm H2O) [16,17]. Each subject received simultaneous electrostimulation of both tibial nerves for the whole duration of one urodynamic cycle and placebo stimulation during the other one. A digital device (TENS/EMS-device EM41; Beurer GmbH, Ulm, Germany) generating biphasic rectangular pulses with a fixed impulse width of 250 ┬Ąsec was used for both types of stimulation: TTNS was performed with an impulse frequency of 20 Hz in contrast to 100 Hz for placebo stimulation. The impulse intensity was set just below the individual pain threshold but never exceeded 180 mA. The skin was shaved and cleaned before applying adhesive electrodes. Fig. 2 shows the transcutaneous electrode placement in both setups. The correct electrode placement for TTNS was verified by either motoric (toe flexion) or sensory response (plantar tingling sensation). This specific placebo stimulation technique was derived from the works of Peters, Chen, and Sharan, aiming to differ as much from TTNS as possible while still being similar enough to successfully blind the subjects [18-20]. To balance both study groups, the order of the verum and placebo stimulations was determined by drawing one out of 50 lots and by coin toss for the 51st test subject. The patients were blinded to the type of stimulation they received in each cycle to meet the requirements of a crossover-controlled trial.
IBM SPSS Statistics ver. 23.0 (IBM Co., Armonk, NY, USA) was used for statistical analysis. The Shapiro-Wilk test showed that most of the gathered data were not normally distributed, which is why mainly nonparametric tests were used for further evaluation. The chi-square and Wilcoxon tests were applied to assess overall changes in urodynamics between TTNS and placebo stimulation. For subgroup analyses, the Mann-Whitney U-test and the Kruskal-Wallis test were used. Linear, inverse, quadratic, and exponential regression analyses were performed. Results are described by median values and interquartile ranges (IQRs) rather than mean values and standard deviation to improve statistical accuracy. The baseline urodynamic values were defined as equal to the gathered data during placebo stimulation; therefore, differences during TTNS are described as improvement or deterioration from baseline.
As shown in Table 1, the participants had a mean age of 62.7┬▒ 15.7 years. About 61% were female and mean body mass index was 28.0┬▒6.3 kg/m┬▓. Around 61% of all participants had been diagnosed with OABS and approximately 47% suffered from urinary stress incontinence. Seventeen patients showed mixed symptoms of urinary incontinence (MUI). Two subjects suffered from reflex incontinence due to a neurologic condition. Recurrent urinary tract infections were reported by roughly 43% of participants. A neurogenic origin of bladder dysfunction (e.g., multiple sclerosis) had either been verified or was at least assumed to be highly probable in about 35% of all cases. The symptoms of the remaining 65% were considered as of traumatic, iatrogenic, or idiopathic origin. Around 65% had already undergone surgical procedures involving the urethra, bladder, prostate, or uterus. A previous LUTS-specific pharmacologic treatment was reported by 49% of all subjects. Further examination revealed signs of anatomical pathology regarding the lower urinary tract (e.g., cystocele or prostate enlargement) in nearly 53% of all participants. Collectively, the standardised questionnaires showed mid-level scores. The median total I-QoL-score was 51 out of 100 (IQR, 32ŌĆō74). The median ICIQ-SF 2004 score was 9 out of 21 (IQR, 0ŌĆō15), the median quality of life 5 out of 10 (IQR, 3ŌĆō7), and the median OABSS was 9 out of 15 (IQR, 3ŌĆō11). Female participants had significantly worse scores than men (e.g., ICIQ-SF 2004: 14 vs. 4, P=0.01) but the perceived quality of life remained comparable between both sexes. Bladder diary analysis showed that significantly fewer male patients suffered from urinary urgency (40% vs. 74%, P=0.02). The fact that those standardized questionnaires mainly focus on incontinence-related questions might explain why women scored significantly worse than men.
The median duration of TTNS was 19 minutes and placebo stimulation was applied during the first urodynamic cycle in 51% of cases. Eleven patients were unable to empty their bladder during urodynamic testing. Coughing and abdominal pressure triggered stress incontinence in 8 patients; DOA was detected in 16 cases. Fourteen participants used their abdominal muscles during placebo stimulation for bladder voiding, but only 12 people needed additional abdominal pressure under the influence of TTNS to empty their bladder. The only reported side effect of transcutaneous electrostimulation was painless flushing at the stimulation site. This was detected immediately afterwards and none of the 5 affected test subjects required any further treatment.
The general statistical analysis showed a widespread distribution of the measured urodynamic values. The median values under the influence of placebo stimulation exceeded the reference range from the literature in several cases [16,17]. Despite the large IQRs, there still were several statistically significant changes under the influence of TTNS. Table 2 shows detailed data for the following findings.
In the entire study sample, there was a significant difference in bladder volume at FDV between TTNS (median, 264 mL) and control (median, 250 mL). The median individual increase (TTNS minus placebo) was 30 mL (P=0.048). When exposed to TTNS, bladder compliance showed a median increase of 3 mL/cm H2O (P=0.01). However, the difference in maximum cystometric capacity (+22 mL during TTNS compared to control) did not reach statistical significance (P=0.07). While 13 subjects showed pathological amounts of postvoid residual during placebo stimulation, there were only 9 persons with postvoid residuals above 100 mL during TTNS (P=0.28).
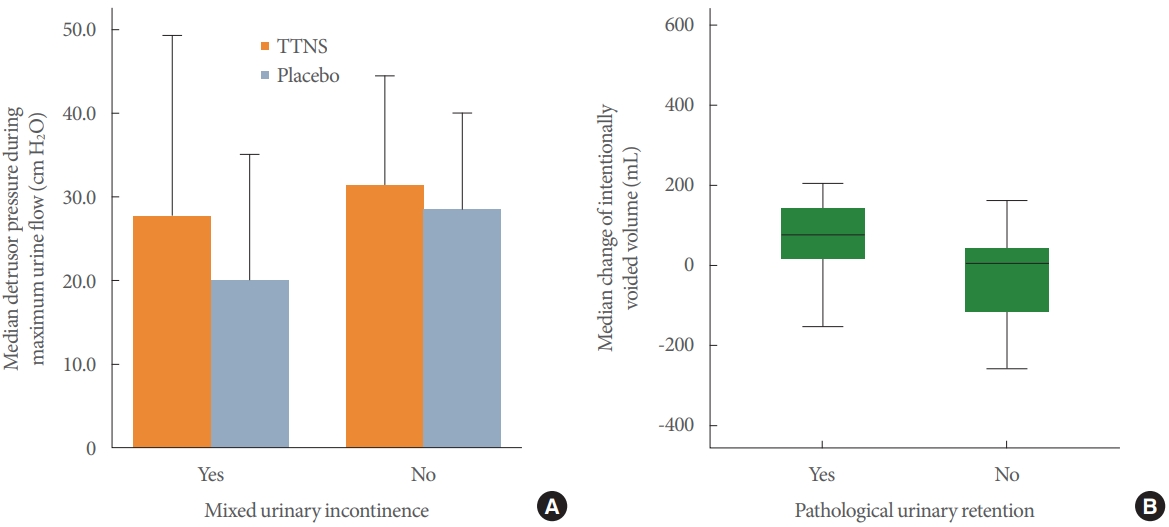
Subgroup analysis showed no statistical difference in urodynamic changes between both sexes. Age and body mass index also had no statistically significant impact on urodynamic results. However, linear regression found a significant difference in bladder volume at first sensation of bladder filling and the individual OABSS. When exposed to TTNS, a high OABSS was related to a large increase in bladder volume at first filling sensation Thus, about 9.7% of the value distribution could be attributed to symptom severity as measured by the OABSS (P= 0.02). Two substantial differences were revealed by building study groups based on their medical conditions (OABS, DOA, stress incontinence, MUI, and urinary retention): Median detrusor pressure during maximum urine flow increased in patients who suffered from MUI by 9 cm H2O (P=0.04), whereas test subjects without MUI showed no change during TTNS. Subjects who suffered from urinary retention had an increase in their voiding volume during TTNS by a median of 76 mL (P=0.03), while voiding volume remained nearly constant for participants without urinary retention. These findings are depicted in Fig. 3. There were no notable urodynamic changes between TTNS and placebo stimulation regarding solely stress incontinence or a potential neurogenic cause. As opposed to this, patients who did not show any sign of anatomical pathologies displayed several significant changes when exposed to TTNS: Their bladder volume at FDV increased by a median of 54 mL (P<0.01). Maximum cystometric capacity grew by 41 mL (P=0.02) and bladder compliance rose by 7 mL/cm H2O (P<0.01). In contrast, the subgroup of patients with anatomical pathologies of the lower urinary tract did not exhibit any remarkable differences.
Verification of correct electrode placement failed in 13.7% of study participants because electrostimulation triggered neither a motoric nor sensory response. However, these patients still showed a significant increase in bladder compliance under the influence of TTNS (median, 6 mL/cm H2O; IQR: 1ŌĆō9; P = 0.047). As a validation of the single-blinded cross-over-setup, every test subject was interviewed after completion of the second urodynamic cycle about whether he or she believed that placebo stimulation had been applied at first. This question was answered correctly by 45.1% of participants, but there was no notable correlation with their urodynamic outcomes. Since urodynamic testing was performed in close succession, the study setup was also checked for potential carryover effects between TTNS and control, but there were no statistically significant differences between patients who received TTNS-first and those who received placebo stimulation first.
After trial completion, 80.4% of participants deemed TTNS a feasible method for daily self-application. Four patients showed an exceptional improvement of their urodynamic parameters during the trial and therefore received instructions to apply bilateral TTNS to themselves at home every day for 30 minutes. A follow-up phone interview was held after 8 weeks: One patient described substantial symptom improvement due to TTNS and was eager to continue TTNS treatment. Another patient reported an initial improvement, but it was not sustained. The other 2 patients had not tried TTNS yet because of other treatment options.
Compared to placebo stimulation, bilateral TTNS induced statistically significant improvements in bladder function. Hence its immediate effectiveness, regardless of the patientŌĆÖs sex, age, and weight, was clinically proven by 3 main findings:
First of all, benefits from TTNS were only found in participants whose lower urinary tract was not affected by anatomical pathologies. Even though some significant urodynamic changes were observed in the entire study sample, a subgroup analysis revealed this to be a statistical fallacy. Considering its postulated mechanism of action, it seems reasonable that TTNS has no effect on structural conditions like bladder outlet obstruction or stress urinary incontinence [7]. This underlines the importance of thorough diagnostics and strict patient selection for neuromodulation.
Secondly, TTNS diminishes bladder sensitivity while increasing its cystometric capacity. Subjects experienced a delay of their FDV by a median of 54 mL. Since most patients who suffer from OABS or urinary incontinence tend to go to the bathroom as soon as they notice a desire to void, this finding ultimately results in a reduction of daytime voids and quality of life consequently improves, just as described by S├©ze et al. [8]. This improvement even seemed to increase in correlation with OABS symptom severity. Thus, TTNS can be esteemed as a particularly favorable treatment option for OABS [21]. The improvement of maximum cystometric capacity by a median of 41 mL could explain the reported reduction of nocturia. The significant increase of bladder compliance by more than 20% demonstrates a TTNS-induced relaxation of the muscular bladder wall during the bladder filling phase. This could explain why TTNS alleviated urinary incontinence in previous studies [9,10].
Finally, TTNS seems likely to improve intentional bladder voiding, most likely by strengthening voluntary detrusor contractions, resulting in increased voiding volumes. Accordingly, TTNS diminished the number of patients with pathological amounts of postvoid residual by 30%. The intervention, therefore, showed a statistical trend to reduce urinary retention. Patients with MUI also showed a statistically significant improvement of detrusor pressure by roughly 35% during their peak of intentional micturition. TTNS may mediate enhanced coordination of voluntary detrusor contractions. Similar findings have been reported by Kabay et al. [22].
Further analysis proved successful randomization (Table 1) and blinding of test subjects. Even without a local motor or sensory response, electrostimulation still had a beneficial effect on bladder function. Hence, there is no need for effective TTNS to exceed the sensory threshold. The vast majority of patients deemed TTNS to be a viable therapy for daily self-application and it caused no adverse effects of medical importance. This renders TTNS an easy-to-use and safe medical procedure even for elderly individuals in residential care, as stated by Booth et al. [23].
However, the peripheral application of TTNS seems to restrict its therapeutic effectiveness compared to SNM [24]. This might explain why the measured changes of urodynamic parameters were relatively small. Another point is that stimulation was only applied during the urodynamic procedure to prove its immediate impact, although the favorable effects of neuromodulation may be likely to occur delayed or need recurrent treatment sessions to be maximized [7]. There are also several other issues to take into account. First, the individual results in study participants were highly heterogeneous. One reason is thatŌĆöeven in a healthy populationŌĆöurodynamic parameters show a broad distribution because they depend on various biometric, psychosocial, and genetic factors [17,25]. Furthermore, there was no preselection of the study sample based on the particular condition. While diminishing potential selection bias, this also reduced the statistical power because several participants presumably could not respond to electrostimulation.
Additionally, about a fifth of the tested subjects were unable to void their bladder, which means their incomplete urodynamic data limited the power of statistical evaluation. Apart from that, there remain uncertainties concerning stimulation frequencies and validation of the introduced placebo stimulation technique.
In conclusion, compared to placebo, simultaneous bilateral TTNS induced immediate improvements in bladder function, particularly regarding OABS and urinary retention. Hence, this study proved TTNS to be a promising, easy-to-use, and safe treatment option for patients whose lower urinary tract is not affected by anatomical pathologies.
Further studies are therefore required to investigate the remaining issues. In particular, whether bilateral TTNS surpasses unilateral TTNS has not yet been examined. Furthermore, the ideal treatment regimen remains to be discussed. Research with a larger number of participants focused on OABS and special types of neurogenic bladder dysfunction may be beneficial to successfully answer those questions.
ACKNOWLEDGEMENTS
The authors thank the hospital staff of the Caritas St. Josef Medical Centre, Regensburg, Germany, for their sedulous assistance, not only regarding everyday work, but especially in clinical research projects. Of course, the authors are especially grateful to each and every patient who volunteered to participate in our clinical study.
NOTES
Research Ethics
Ethical approval for this clinical trial was obtained from the ethical review committee of the University of Regensburg, Germany, (reference number 16-101-0176) in accordance with the World Medical Association Declaration of Helsinki. The trial (Universal Trial Number: U1111-1245-8723) was registered in the German Clinical Trials Register (DRKS-ID: DRKS00020402) and adhered to the CONSORT statement (www.consort-statement.org). Written informed consent was obtained from all subjects included in this clinical trial.
AUTHOR CONTRIBUTION STATEMENT
┬Ę Conceptualization: FG, HS, MB, RM
┬Ę Data curation: FP, TH, MH, CP
┬Ę Formal analysis: FP, FZ
┬Ę Funding acquisition: HS, MB, RM
┬Ę Methodology: HS, FZ, TH, MH, CP, RM
┬Ę Project administration: HS, MB, RM
┬Ę Visualization: FP, HS, TH, MB, RM
┬Ę Writing-original draft: FP, TH, MH, CP, RM
┬Ę Writing-review & editing: HS, FZ, TH, MH, CP, MB, RM
REFERENCES
1. Del R├Ło-Gonzalez S, Aragon IM, Castillo E, Milla-Espa├▒a F, Galacho A, Machuca J, et al. Percutaneous tibial nerve stimulation therapy for overactive bladder syndrome: clinical effectiveness, urodynamic, and durability evaluation. Urology 2017;108:52-8. PMID: 28687483


2. Dedemadi G, Takano S. Efficacy of bilateral transcutaneous posterior tibial nerve stimulation for fecal incontinence. Perm J 2018;22:17-231. 
3. Sanford MT, Suskind AM. Neuromodulation in neurogenic bladder. Transl Androl Urol 2016;5:117-26. PMID: 26904417


4. McGuire EJ, Zhang SC, Horwinski ER, Lytton B. Treatment of motor and sensory detrusor instability by electrical stimulation. J Urol 1983;129:78-9. PMID: 6600794


5. Peters KM, Carrico DJ, Wooldridge LS, Miller CJ, MacDiarmid SA. Percutaneous tibial nerve stimulation for the long-term treatment of overactive bladder: 3-year results of the STEP study. J Urol 2013;189:2194-201. PMID: 23219541


6. Ram├Łrez-Garc├Ła I, Blanco-Ratto L, Kauffmann S, Carralero-Mart├Łnez A, S├Īnchez E. Efficacy of transcutaneous stimulation of the posterior tibial nerve compared to percutaneous stimulation in idiopathic overactive bladder syndrome: randomized control trial. Neurourol Urodyn 2019;38:261-8. PMID: 30311692


7. Abello A, Das AK. Electrical neuromodulation in the management of lower urinary tract dysfunction: evidence, experience and future prospects. Ther Adv Urol 2018;10:165-73. PMID: 29623108



8. de S├©ze M, Raibaut P, Gallien P, Even-Schneider A, Denys P, Bonniaud V, et al. Transcutaneous posterior tibial nerve stimulation for treatment of the overactive bladder syndrome in multiple sclerosis: results of a multicenter prospective study. Neurourol Urodyn 2011;30:306-11. PMID: 21305588


9. Booth J, Connelly L, Dickson S, Duncan F, Lawrence M. The effectiveness of transcutaneous tibial nerve stimulation (TTNS) for adults with overactive bladder syndrome: a systematic review. Neurourol Urodyn 2018;37:528-41. PMID: 28731583


10. Amarenco G, Ismael SS, Even-Schneider A, Raibaut P, Demaille-Wlodyka S, Parratte B, et al. Urodynamic effect of acute transcutaneous posterior tibial nerve stimulation in overactive bladder. J Urol 2003;169:2210-5. PMID: 12771752


11. Kamboonlert K, Panyasriwanit S, Tantisiriwat N, Kitisomprayoonkul W. Effects of bilateral transcutaneous tibial nerve stimulation on neurogenic detrusor overactivity in spinal cord injury: a urodynamic study. Arch Phys Med Rehabil 2021;102:1165-9. PMID: 33245938


12. Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn 2004;23:322-30. PMID: 15227649


13. Blaivas JG, Panagopoulos G, Weiss JP, Somaroo C. Validation of the overactive bladder symptom score. J Urol 2007;178:543-7. PMID: 17570417


14. Bushnell DM, Martin ML, Summers KH, Svihra J, Lionis C, Patrick DL. Quality of life of women with urinary incontinence: cross-cultural performance of 15 language versions of the I-QOL. Qual Life Res 2005;14:1901-13. PMID: 16155777


15. Rosier PFWM, Schaefer W, Lose G, Goldman HB, Guralnick M, Eustice S, et al. International Continence Society Good Urodynamic Practices and Terms 2016: Urodynamics, uroflowmetry, cystometry, and pressure-flow study. Neurourol Urodyn 2017;36:1243-60. PMID: 27917521


16. Mahfouz W, Al Afraa T, Campeau L, Corcos J. Normal urodynamic parameters in women: part II--invasive urodynamics. Int Urogynecol J 2012;23:269-77. PMID: 22011933



17. Wyndaele JJ. Normality in urodynamics studied in healthy adults. J Urol 1999;161:899-902. PMID: 10022710


18. Chen ML, Chermansky CJ, Shen B, Roppolo JR, de Groat WC, Tai C. Electrical stimulation of somatic afferent nerves in the foot increases bladder capacity in healthy human subjects. J Urol 2014;191:1009-13. PMID: 24113017


19. Peters K, Carrico D, Burks F. Validation of a sham for percutaneous tibial nerve stimulation (PTNS). Neurourol Urodyn 2009;28:58-61. PMID: 18671297


20. Sharan E, Hunter K, Hassouna M, Yoo PB. Characterizing the transcutaneous electrical recruitment of lower leg afferents in healthy adults: implications for non-invasive treatment of overactive bladder. BMC Urol 2018;18:10. PMID: 29439703



21. Gupta P, Ehlert MJ, Sirls LT, Peters KM. Percutaneous tibial nerve stimulation and sacral neuromodulation: an update. Curr Urol Rep 2015;16:4. PMID: 25630918


22. Kabay S, Canbaz Kabay S, Cetiner M, Mestan E, Sevim M, Ayas S, et al. The clinical and urodynamic results of percutaneous posterior tibial nerve stimulation on neurogenic detrusor overactivity in patients with ParkinsonŌĆÖs disease. Urology 2016;87:76-81. PMID: 26436213


23. Booth J, Hagen S, McClurg D, Norton C, MacInnes C, Collins B, et al. A feasibility study of transcutaneous posterior tibial nerve stimulation for bladder and bowel dysfunction in elderly adults in residential care. J Am Med Dir Assoc 2013;14:270-4. PMID: 23206722


24. Tutolo M, Ammirati E, Heesakkers J, Kessler TM, Peters KM, Rashid T, et al. Efficacy and safety of sacral and percutaneous tibial neuromodulation in non-neurogenic lower urinary tract dysfunction and chronic pelvic pain: a systematic review of the literature. Eur Urol 2018;73:406-18. PMID: 29336927


25. Lukacz ES, Sampselle C, Gray M, Macdiarmid S, Rosenberg M, Ellsworth P, et al. A healthy bladder: a consensus statement. Int J Clin Pract 2011;65:1026-36. PMID: 21923844



Fig.┬Ā1.
Flow diagram of trial setup, enrolment, and analysis (based on www.consort-statement.org). TTNS, transcutaneous tibial
nerve stimulation.
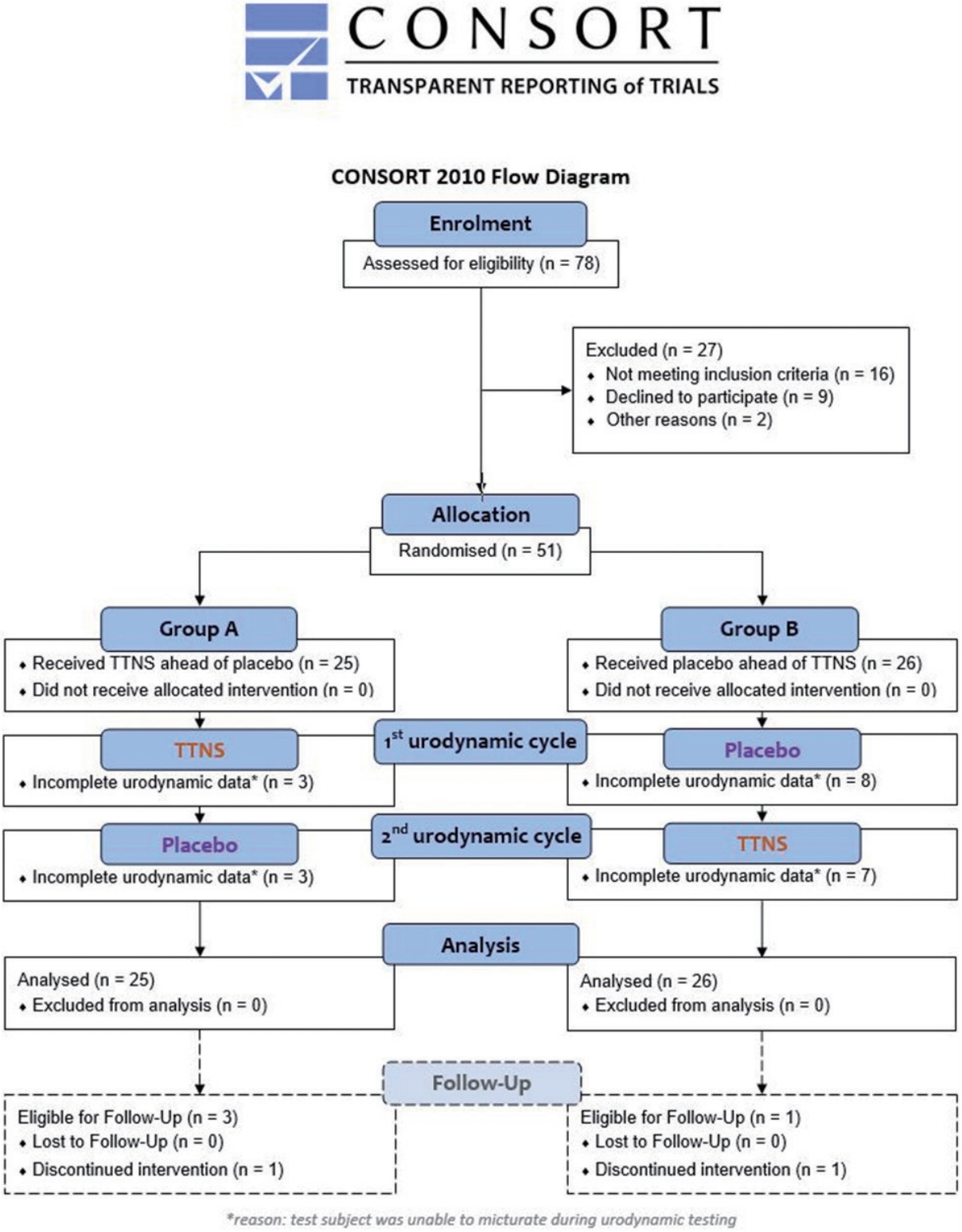
Fig.┬Ā2.
Electrode placement for transcutaneous tibial nerve stimulation (TTNS; A) and placebo stimulation (B).

Fig.┬Ā3.
(A) Changes in median detrusor pressure during maximum urine flow (cm H2O) in patients with and without mixed urinary
incontinence. (B) Median changes of voided volumes (mL) in patients with and without pathological urinary retention. TTNS, transcutaneous tibial nerve stimulation.
Table┬Ā1.
Comparison of biometric data between the entire study sample (N=51), the TTNS-first group (n=25), and the placebo-first group (n=26)
Table┬Ā2.
Summary of urodynamic changes between TTNS and control
TTNS, transcutaneous tibial nerve stimulation; Control, placebo stimulation; IQR, interquartile range; difference TTNS - control, median individual change of value; volume at FDV, bladder volume at first desire to void; Cystometric capacity, maximum cystometric capacity; Compliance, bladder compliance; Qmax, maximum urine flow rate.





