Transitional Urology in Korea: Initial Insights Through a Cross-Sectional Study
Article information
Abstract
Purpose
In Korea, the field of transitional urology (TU) is in its nascent stages, with its introduction only beginning. This study aims to evaluate the existing state of TU prior to implementing a transition protocol, and to identify key areas of focus for the development of an effective transition protocol.
Methods
From June 1, 2021 to May 31, 2023, clinical data were retrospectively collected for patients who visited the adult urology or pediatric urology outpatient departments of this hospital and were aged 10 or older, with medical conditions falling under the category of TU. We analyzed the patient distribution across different disease groups. The transitional stages were categorized from T1, indicating initial care by pediatric urologists, to T4, denoting complete transition to adult care. ‘T4x’ was used for patients with unknown medical histories, and ‘T4only’ for those who had never been under pediatric urology care.
Results
During a 2-year period, a total of 1,484 patients received outpatient care for diseases in TU field. The most prevalent diseases were hypospadias (40.4%), spinal bifida (37.3%), and congenital ureteral anomalies (17.7%), with other conditions accounting for 4.6%. Among 553 spinal bifida patients, only 5.3% completed transitional care (T4), while 80.1% were in the initial phase (T1). For patients introduced to adult urology (T2–T4), 37.7% reached T4, highlighting a marked increase in transition completion within this subset (P<0.001).
Conclusions
TU in Korea is in its nascent stage, with a significant gap in the initiation and completion of transitional care for patients with congenital urologic conditions. Early initiation and active engagement in transitional care are crucial for successful transition. This study highlights the need for structured transition protocols to address the complex needs of this patient population.
INTRODUCTION
With the advancements in the treatment and management of pediatric urology and congenital diseases, the field of transitional urology (TU) has taken on an increasing importance in recent years as more individuals with congenital urologic issues are living and thriving into adulthood [1, 2]. Patients have a strong desire for being “normal” and, considering that they have to live the remaining lifespan with their condition, it is crucial to clearly define the limitations and goals that can be reached and provide assistance in any possible aspect. The complexity and challenging management associated with congenital diseases have emphasized the need for transitional urologists [3]. However currently there’s a scarcity of urologists specializing in TU. and notably, there are no formal training programs available within any healthcare system specifically designed to train transitional urologists. In Korea, TU is just beginning to be introduced in its initial stages. Recognizing the growing importance of TU, a preliminary study is needed before creating a transition protocol and transitional clinic at any institution. The purpose of this study are to analyze the current state of transitional care, to determine the prevalence of diseases in TU, and to determine the incidence of transitional stages of spinal bifida (SB) so as to determine which aspects should be emphasized first in setting up the future transition protocol.
MATERIALS AND METHODS
Study Population
This study was conducted from June 1, 2021 to October 1, 2023. Medical records of all patients aged 10 and above who visited our institution with conditions pertaining to TU were reviewed. 10 years of age is the age at which transition takes place. Although there is controversy over the best time to begin transitional care, the decision to use 10 years old as the inclusion criteria in the study was made to gather the widest range of patient groups. The distribution of patients by each disease group was analyzed. The current set-up in our institution is a separate adult and urology department coexisting independently. The 2 departments collaborate weekly through conferences to discuss patients with congenital urological problems.
A subset analysis of patients with SB was done because it is the most frequently and actively discussed in conferences. Their current transition stages were analyzed.
Range of TU
The disease groups in TU were classified as follows: (1) SB, (2) hypospadias (HS), (3) epispadias or exstrophy (EPI), (4) congenital ureteral anomaly including ectopic ureter, vesicoureteral reflux, and obstructive uropathy (CUA), (5) posterior urethral valve (PUV), (6) cloacal malformation (CM), (7) disorders of sexual development (DSD), and (8) prune belly syndrome (PB). Patients were classified according to their primary diagnosis, and those with overlapping diseases were categorized into one group based on the disease that presents the main clinical problem. Vesicoureteral reflux is included in the CUA group, but adult secondary or non-congenital vesicoureteral reflux was excluded from the study.
Transition Stage
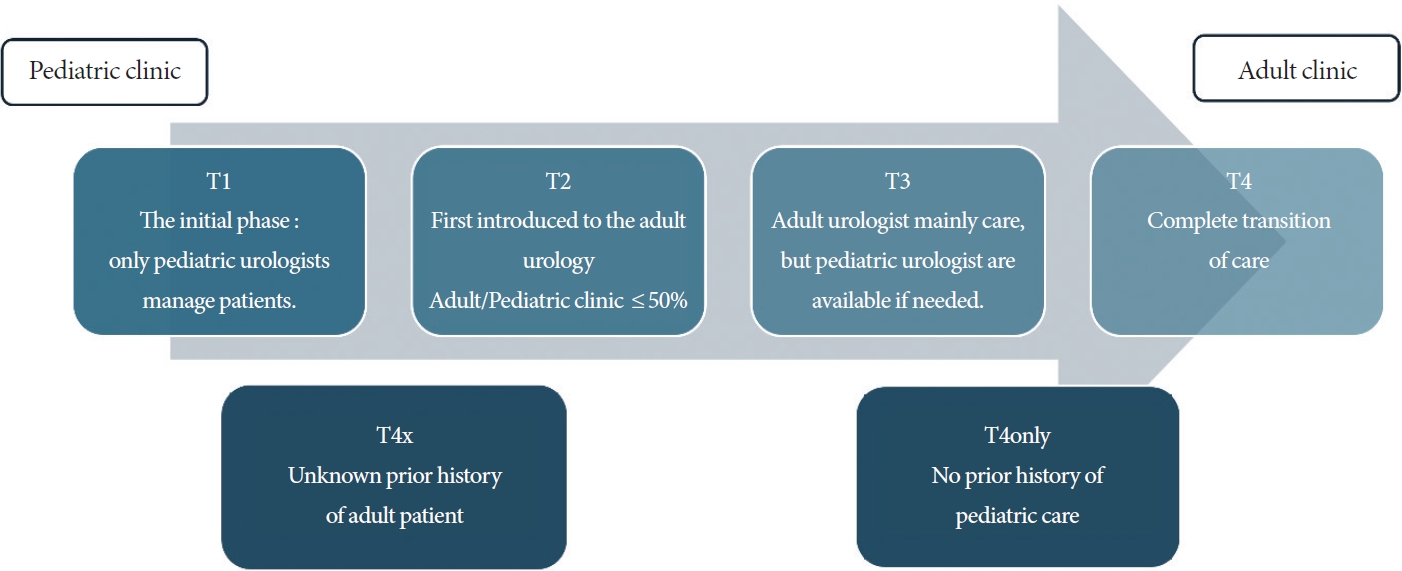
Transition stages are helpful in understanding the current status and condition of transition for individual patients and serve as a useful indicator for the overall status of transition at the center. In this study, transition stages used were adapted from the transitional stages presented by Blubaum et al. [4]. Transition stages in this study were defined as follows (Fig. 1): T1 represents the initial phase of transitional care when patients are still receiving management from only pediatric urologists. T2 marks the introduction to adult urology for the first time. T3 denotes primarily receiving care from adult urologists while still requiring assistance and consultations from pediatric urologists. T4 designates the completion of transitional care. T4x indicates cases where the previous medical history is unknown, while T4only applies to individuals who have never visited a pediatric urologist. Outpatients visit records and medical records of patients were reviewed to determine their current stage of transition.
Statistical analyses were conducted using IBM SPSS Statistics ver. 23.0 (IBM Co., Armonk, NY, USA). Descriptive statistics were used to represent patient characteristics and clinical information. We calculated the proportion of transitional completion (T4) in the entire group as well as in the subset of patients who were introduced to the adult urology department (T2, T3, T4). To test the difference in proportions between the 2 groups, we used the chi-square test. A P-value of less than 0.05 was defined as statistically significant.
RESULTS
A total of 1,484 patients received outpatient care for diseases in TU field. The mean age was 17.3±9.9 years, with a ratio of male to female of 1,101:383. The most common conditions in descending order were HS (40.4%), SB (37.3), and CUA (17.7%) as shown in Fig. 2. Other conditions, including EPI, PUV, CM, DSD, and PB, all together accounted for 4.6%, showing a frequency of less than 5%.

Patient distribution for each disease group corresponding to transitional urology. SB, spinal bifida; HS, hypospadias; EPI, epispadias or exstrophy; CUA, congenital ureteral anomaly including ectopic ureter, vesicoureteral reflux, and obstructive uropathy; PUV, posterior urethral valve; CM, cloacal malformation; DSD, disorders of sexual development; PB, prune belly syndrome.
In subset analysis, a total of 553 patients are in the SB group, the distribution of transitional stages is illustrated in Fig. 3A. When analyzing transitional stage, only 29 patients (5.3%) achieve completion of transition stage (T4), while a significant number, 443 patients (80.1%), were not yet introduced to the adult urology department (T1). However, among the patients who were already introduced to adult urology, corresponding to transitional stages T2, T3, and T4, the proportions were 49.3%, 13.0%, and 37.7% respectively, as shown in Fig. 3B. Notably, the proportion of T4 was significantly higher in the T2-T4 group compared to that in the entire population (P<0.001).

(A) Transitional stages of SB group patients. (B) Transitional stages only for patients who were once introduced to the adult clinic (T2–T4). SB, spinal bifida. T1, the initial phase: only pediatric urologists manage patients; T2, first introduced to the adult urology, adult/pediatric clinic ≤50%; T3, adult urologist mainly care, but pediatric urologist are available if needed; T4, complete transition of care; T4x, unknown prior history of adult patient; T4only, no prior history of pediatric care.
DISCUSSION
In this study, we observed that patients in the TU primarily belong to 2 groups: HS and SB. Together, these groups constitute 77.7% of the patient population. with more than three-quarters of patients falling into these categories. Considering that these patients constitute more than three-quarters of patients, when first starting a transitional clinic, it might be a good strategy to focus on these most common disorder groups. Once the transitional clinic is set up, it can then expand its scope to other disease groups.
The most notable finding in transitional stage analysis is that 80.11% of patients in the SB group remain at the transitional stage T1. T1 represents patients who have not yet fully commenced the transition and are only receiving care in pediatric urology. This indicates that the initiation of transitional care is not occurring properly. On the other hand, when considering only the patients after being introduced to adult urology (T2–T4), it is observed that T4 appeared at a significantly high proportion of 37.7% (P<0.001). Hence, for institutions implementing a transitional clinic for the first time, it is crucial to prioritize initiating transitional care with patients, thereby progressing beyond the initial T1 stage. Therefore, in the transition protocol, the process of explaining the importance of transitional care to patients and their guardians through detailed and patientfriendly explanations and persuading them should be emphasized.
Transitional care is a challenging process. The barriers to transition can be categorized into 3 types: patient and family level barriers, provider level barriers, and system level barriers [5-7]. Patient and family level barriers include personal preferences such as whether the patient or family actively desires the transition or prefers to remain in the pediatric urology department. The desire of each patient for transitional care can determine the success of the transition regardless of medical complexity [8, 9]. Provider level barriers include the absence of a transition clinic, lack of a transition protocol, absence of transitional urologist specialists and training, and the absence of appropriate guidelines [2]. System level barriers relate to socioeconomic aspects, including health insurance, additional costs for patient care and treatment, and socioeconomic institutional support. Since this study focuses on a single institution, it is presumed that system level barriers had a lesser impact, and the analysis suggests that provider level barriers, primarily due to the lack of an appropriate protocol, were more influential.
Despite the various barriers in TU, it is still important. The greatest loss from a failure to transition properly is the preventable loss of function. Additionally, a successful transition allows patients: (1) to move from being dependent on others for decision-making to making own independent decisions and (2) to engage more actively in their treatment. There have been reports that groups with successful transitions have significantly lower emergency department visit rates [8]. Additionally, it has been reported that patients who did not undergo adequate transition had higher rates of emergency department visits, hospitalization, and surgical costs [10]. In a survey conducted by O’Kelly et al. [11] among pediatric urologists worldwide, about 93% of respondents answered that the importance of TU was either important or extremely important, acknowledging that TU is a field that is essential for the future.
Over the past decade, transitional care units have been established in various countries [12]. Several institutions have applied transitional protocols and reported their outcomes. In the United States, several institutions have shared their experiences and results from years of operating transition clinics [4, 8, 13, 14]. Szymanski et al. [8] reported their 7-year experience with an SB multidisciplinary transition team, noting that about 40% of patients achieved a successful transition. Similarly, there are reports on transitional clinics and their outcomes and detail experiences in Europe as well [9, 15]. However, in Asia, there are no reports yet on transitional clinics, and in South Korea, the field of TU is only beginning to attract interest and adoption. With socioeconomic development, there is a shift in focus towards quality of life rather than just survival, leading to increased attention on patients with pediatric and congenital urologic conditions. As previously mentioned, the importance of transitional care is well recognized, highlighting the need for its swift implementation.
The appropriate age for transition is another point of discussion. It is recommended that the transitional process should begin before the age of 12 and that appropriate transitions are made by the age of 18, when patients receive most of their care in the adult urology department, but there is still no consensus on the exact age cutoff [16]. In a study by O’Kelly et al. [11], a survey conducted among pediatric urologists worldwide asked about the appropriate age for transition; 23.8% responded 11–13, 38.4% said 13–15, 29.6% chose 15–17, and 8.7% indicated 17–19. Given the diversity in transitional issues and congenital problems among patients, customized approach to determine the appropriate age to begin transition, rather than setting a numerical cutoff value, is advisable. Puberty marks the second most dramatic period of physical change, with hormonal changes, bladder function, sexual function, and other changes. Researching the correlation between pubertal stage and the optimal transition age would be logical. However, the importance of starting transition early and the ease with which earlier exposure facilitates adaptation to transition suggest that introducing transitional care before the age of 12 could increase the likelihood of a successful transition.
For effective transitional care, multidisciplinary medical teams are essential [5, 7]. For instance, managing SB requires collaboration among neurosurgeons, orthopedists, physiatrists, and physical therapists. Similarly, CM necessitate the cooperation of colorectal surgeons and specialists in gynecology and obstetrics, while DSD call for a team including gynecologists, obstetricians, endocrinologists, fertility specialists, and psychologists [5]. Not only adult and pediatric urologists but also various other department must collaborate to provide appropriate care to patients with complex histories and issues. In this context, South Korea faces issues with the medical fees for multidisciplinary care, necessitating policy changes to enable smoother implementation of such care.
This study has several limitations. First, as a cross-sectional study, it collects data at a specific point in time, which limits the ability to determine causality. Therefore, it is not possible to know the exact relationship of what factors influence the transition protocol and quantitative analysis is also impossible. As a preliminary study, only a superficial analysis could be conducted, and the causal relationship regarding which aspect of the transitional barrier has the most significant impact remains unclear. Second, as a single-institution study, there is a potential for selection bias. In our institution, there is a significantly higher concentration of patients with HS compared to the typical case, which differs from the general distribution of diseases in TU. Despite these limitations, this study holds significant importance as it demonstrated the difficulties of transition and the critical importance of introducing and initiating transitional care and it is the first study on TU conducted in Korea.
In conclusion, transitional care in urology aims to transition patients with congenital urologic anomalies from pediatric care to adult care, addressing a significant number of patients with complex and challenging issues. The fact that 80% of cases in SB have not even started transitional care highlights the difficulty of transition in the absence of a transitional protocol. On the other hand, the rate of transition completion was significantly higher in patients who had been introduced to the adult clinic at least once, suggesting that the initiation of transition is the most important aspect in the setting of a transition protocol. It is necessary to change the perspectives of patients and their parents through adequate explanation and education, enabling them to actively engage in transitional care.
Notes
Grant/Fund Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Research Ethics
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Yonsei University College of Medicine (4-2023-1044). The Institutional Review Board of Yonsei University College of Medicine waived the requirement of obtaining informed consent because this study retrospectively reviewed anonymous patient data and did not include the use of human tissue samples.
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTION STATEMENT
· Conceptualization: KTO, JHK
· Data curation: KTO, ANL, ARI
· Formal analysis: KTO
· Methodology: KTO, ANL, ARI
· Project administration: JHK
· Visualization: KTO
· Writing - original draft: KTO
· Writing - review & editing: ANL, JHK