Surgical Outcomes and Predictive Factors in Patients With Detrusor Underactivity Undergoing Bladder Outlet Obstruction Surgery
Article information
Abstract
Purpose
This study was conducted to evaluate the efficacy of bladder outlet surgery in patients with detrusor underactivity (DU) and to identify factors associated with successful outcomes.
Methods
We conducted a retrospective review of men diagnosed with DU in urodynamic studies who underwent bladder outlet surgery for lower urinary tract symptoms between May 2018 and April 2023. The International Prostate Symptom Score (IPSS) questionnaire, uroflowmetry (UFM), and multichannel urodynamic studies were administered. Successful treatment outcomes were defined as either an IPSS improvement of at least 50% or the regaining of spontaneous voiding in patients urethral catheterization prior to surgery.
Results
The study included 93 male patients. Men diagnosed with significant or equivocal bladder outlet obstruction (BOO) experienced significant postoperative improvements in IPSS (from 20.6 to 6.0 and from 17.4 to 6.5, respectively), maximum urine flow rate (from 5.0 mL/sec to 14.4 mL/sec and from 8.8 mL/sec to 12.2 mL/sec, respectively) and voiding efficiency (from 48.8% to 86.0% and from 61.2% to 85.1%, respectively). However, in the group without obstruction, the improvements in IPSS and UFM results were not significant. The presence of detrusor overactivity (odds ratio [OR], 3.152; P=0.025) and preoperative urinary catheterization (OR, 2.756; P=0.040) were associated with favorable treatment outcomes. Conversely, an unobstructed bladder outlet was identified as a negative prognostic factor.
Conclusions
In men with DU accompanied by equivocal or significant BOO, surgical intervention to alleviate the obstruction may enhance the IPSS, quality of life, and UFM results. However, those with DU and an unobstructed bladder outlet face a comparatively high risk of treatment failure. Preoperative detrusor overactivity and urinary catheterization are associated with more favorable surgical outcomes. Consequently, active deobstructive surgery should be considered for patients with DU who are experiencing urinary retention.
INTRODUCTION
Bladder outlet deobstructive procedures, such as transurethral resection of the prostate (TURP) or laser prostatectomy, are effective in treating voiding dysfunction that is refractory to medical treatment [1,2]. However, the efficacy of deobstructive surgery may differ among patients with detrusor underactivity (DU) [3-5]. This condition is characterized by contractions of reduced strength and/or duration, leading to prolonged bladder emptying and/or the inability to achieve complete emptying within a typical timeframe [6]. The variability in research findings regarding these surgical procedures may stem from certain factors that have been overlooked, such as the presence and severity of bladder outlet obstruction (BOO). However, few studies have explored prognostic factors in these cases. The present study was conducted to assess the efficacy of surgical intervention for BOO in patients with DU, as well as to identify factors associated with postoperative success. This was achieved by integrating preoperative clinical data with comprehensive urodynamic assessments. The ultimate objective was to identify suitable candidates for surgery and consequently enhance surgical outcomes.
MATERIALS AND METHODS
We conducted a retrospective review of patients diagnosed with DU, characterized by a bladder contractility index (BCI) of less than 100 in a preoperative pressure-flow study, who underwent surgery for BOO at our institution from May 2018 to April 2023. We excluded patients with urethral stricture, those who had undergone repeated surgery for BOO, and those with a clear neurogenic bladder etiology, including spinal cord injury and multiple sclerosis. Prior to surgery, all patients underwent a baseline assessment of lower urinary tract function, which included uroflowmetry (UFM), a postvoid residual (PVR) urine test, and a multichannel urodynamic study. The multichannel urodynamic study, consisting of filling cystometry and a pressure-flow study, was conducted preoperatively in accordance with International Continence Society recommendations for good urodynamic practice [7]. UFM parameters such as voided volume (VV), maximum flow rate (Qmax), bladder capacity, and voiding efficiency were obtained from the UFM and PVR data. Bladder capacity was calculated as the sum of VV and PVR, while voiding efficiency was determined by dividing VV by bladder capacity. During the multichannel urodynamic study, we recorded bladder sensation, compliance, and the presence of detrusor overactivity (DO) as filling phase parameters. Voiding phase parameters included detrusor pressure at maximum flow rate (PdetQmax), Qmax, VV, bladder capacity, and PVR. We stratified patients using the bladder outlet obstruction index (BOOI), calculated as PdetQmax−2Qmax [8], with a BOOI greater than 40, which is generally accepted as indicative of clinical obstruction in men. Equivocal obstruction was defined as a BOOI between 20 and 40.
All patients underwent surgery for BOO, with procedures including TURP, GreenLight photoselective vaporization of the prostate (GLPVP), and transurethral incision of the bladder neck (TUIBN). Three months postoperatively, the International Prostate Symptom Score (IPSS) questionnaire, UFM, and PVR testing were administered. Treatment success was defined as a reduction in the total IPSS of at least 50% compared to baseline or the restoration of spontaneous voiding in patients who required urinary catheterization before surgery.
Data and Statistical Analysis
Statistical analyses were performed using IBM SPSS Statistics ver. 25.0 (IBM Co., Armonk, NY, USA). Continuous variables are presented as mean±standard deviation, while categorical variables are expressed as numbers and percentages. For statistical comparisons between groups, the Kruskal-Wallis and Mann-Whitney U-tests were employed for continuous variables, while the chi-square and McNemar tests were used for categorical variables. The Fisher exact test was applied when more than 20% of the expected frequencies were less than 5. Within-group differences between baseline and follow-up were analyzed using the paired t-test for continuous variables and the McNemar test for categorical variables. Univariate and multivariate logistic regression analyses were utilized to identify potential predictors of treatment success. A 2-tailed P-value of less than 0.05 was considered to indicate statistical significance for all analyses.
RESULTS
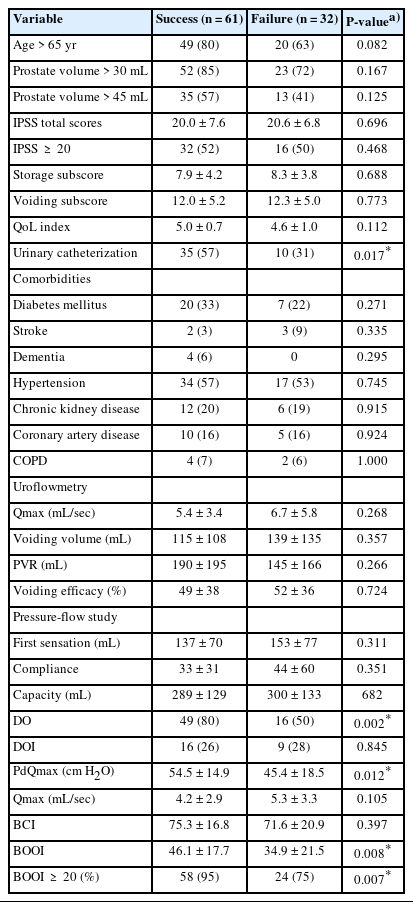
The study included a total of 93 male patients. The demographics of participants who underwent TURP, GLPVP, and TUIBN are detailed in Supplementary Table 1. Of these patients, 49 (52.7%) had significant BOO, 33 (35.5%) had equivocal BOO, and 11 (11.8%) had no obstruction. Regarding urodynamic parameters, the presence of DO during the storage phase, mean PdetQmax, and BCI all decreased progressively with lower grades of BOO. A lower Qmax was observed among those with significant obstruction compared to the equivocally obstructed and unobstructed groups. The clinical baseline demographics and preoperative urodynamic parameters, stratified by BOOI, are presented in Table 1.
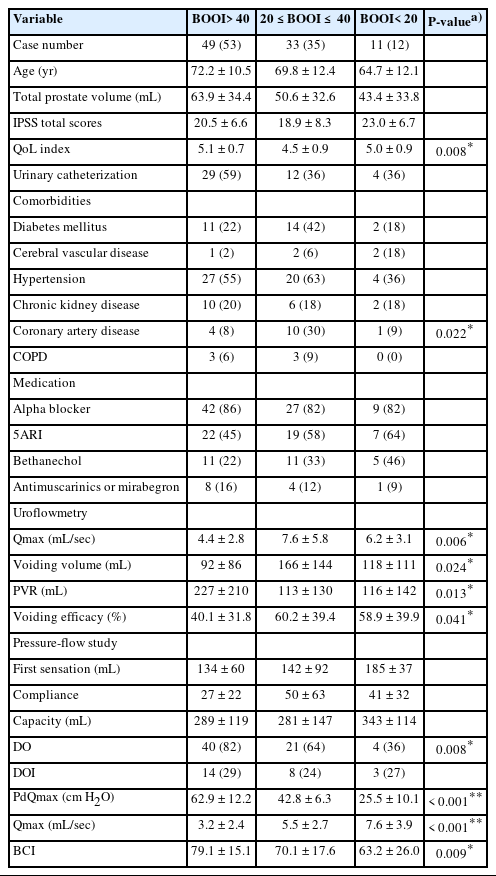
Baseline demographics and urodynamic parameters in patients with detrusor underactivity stratified by bladder outlet obstruction index (BOOI)
Table 2 summarizes the therapeutic outcomes among patients with DU who underwent surgery for BOO, categorized by BOOI. Both the IPSS—which included the total score, storage subscore, voiding subscore, and quality-of-life index—and each parameter showed significant improvement after surgery in the group with obstruction (all P<0.05). UFM parameters also significantly improved following surgery, with VV increasing from 115 mL to 170 mL (P=0.017), Qmax improving from 5.0 mL/sec to 14.4 mL/sec (P<0.001), PVR decreasing from 204 mL to 44 mL (P<0.001), and voiding efficiency improving from 48.8% to 86.0% (P<0.001), in patients who presented with significant BOO. Conversely, among the patients without obstruction, improvements in IPSS and UFM were not significant apart from Qmax, which increased from 6.9 mL/sec to 14.7 mL/sec (P=0.039). Among the patients with obstruction, the proportions requiring α-blockers and 5α-reductase inhibitors significantly decreased after surgery, from 86% to 22% (P<0.001) for α-blockers and from 45% to 16% (P=0.003) for 5α-reductase inhibitors. A similar trend was observed in the equivocal group, with the proportion of patients taking α-blockers dropping from 82% to 15% (P<0.001) and those on 5α-reductase inhibitors falling from 58% to 9% (P<0.001). However, no significant postoperative reduction in the use of these medications was observed among the patients with no obstruction.

Changes of subjective and objective parameters at baseline and at follow-up in patients with detrusor underactivity stratified by bladder outlet obstruction index (BOOI)
Table 3 presents the preoperative clinical characteristics and multichannel urodynamic parameters of the patients who underwent surgery for BOO, categorized by treatment outcome. Of these patients, 61 (65.6%) experienced an IPSS reduction of at least 50% or regained spontaneous voiding within 3 months following surgery. The patients with successful outcomes displayed significantly higher DO prevalence (80% vs. 50%, P=0.002), PdetQmax (54.5 cm H2O vs. 45.4 cm H2O, P=0.012), and BOOI (46.1 vs. 34.9, P=0.008) compared to those with unsuccessful treatment. No significant differences were observed in baseline IPSS score, Qmax, PVR, or voiding efficacy prior to surgery. Multivariate analysis indicated that the presence of DO (odds ratio [OR], 3.152; P=0.025) and preoperative urethral catheterization (OR, 2.756; P=0.040) were associated with favorable treatment outcomes. Conversely, an unobstructed bladder outlet was identified as a factor negatively associated with treatment success (OR, 4.599; P=0.049) following surgery for BOO (Table 4).
DISCUSSION
The benefit of bladder outlet surgery for the treatment of lower urinary tract symptoms in patients with DU is unclear. Our study revealed that 66% of these patients reported subjective improvement following bladder outlet surgery. BOOI represented a key prognostic factor. Patients with positive or equivocal BOO experienced benefits from deobstructive surgery, whereas those without obstruction did not show significant improvement. Additionally, the presence of DO and the preoperative use of urethral catheterization were favorable prognostic indicators for patients with DU undergoing bladder outlet surgery. These findings suggest that careful patient selection could optimize the outcomes of bladder outlet surgery in clinical practice.
Several explanations have been proposed for DU [9,10]. One theory suggests that DU may arise from bladder decompensation following chronic BOO caused by collagen deposition within the bladder wall. This accumulation leads to progressive bladder fibrosis and a subsequent reduction in bladder contractility [10,11]. Outcomes of deobstructive surgery among patients with DU have been inconsistent. Some studies have reported IPSS improvements, benefits to urine flow, or restoration of spontaneous voiding after surgery [12-15]. In contrast, other research indicates that patients with DU are less likely to see improvements or may even experience worse outcomes following surgery compared to those without DU [4,16]. The variability in surgical outcomes may stem from differing definitions of treatment success. Although improvements after deobstructive surgery were less pronounced among patients with DU than in those without this condition, they were still significant [16-18]. Furthermore, not all studies have reported the proportion of patients who did not have BOO. Logic indicates that patients without BOO may not benefit from deobstructive surgery.
BOOI is a key predictor of operative outcomes in patients undergoing surgery to alleviate prostate obstruction [19]. It has also been identified as an important parameter in patients with DU who undergo deobstructive surgery [20,21]. BOO is implicated in complex cases of voiding dysfunction, and alleviating the obstruction can partially address this condition. Additionally, a higher BOOI may indicate a relatively early stage of bladder decompensation, which preserves more bladder contractility relative to patients without obstruction. Patients with higher BOOI may therefore benefit from early correction of BOO, before bladder decompensation occurs [9]. However, further research is necessary to validate the 3-stage model hypothesis and to ascertain the optimal timing for surgical intervention in patients with BOO. Deobstructive surgery may offer minimal benefit to patients without obstruction, as BOO is not a primary cause of voiding dysfunction.
The role of DO in bladder outlet surgery remains a subject of debate. Liu et al. [22] and the present findings indicate that preoperative DO is a positive prognostic factor in patients with DU undergoing bladder outlet surgery. In contrast, a recent meta-analysis found no correlation between preoperative DO and surgical outcomes in male patients with BOO [23]. Moreover, a large-scale study demonstrated that both age and BOO are independently associated with the presence of DO [24]. DO may represent a secondary response of the bladder to BOO during the compensated phase, and surgical relief of the obstruction may reverse DO along with symptoms of overactive bladder [9,25,26]. This could account for our observation that patients with preoperative DO experienced better outcomes than those without DO. Further research is necessary to elucidate the impact of preoperative DO on the results of bladder outlet surgery.
Regaining spontaneous voiding is often the primary goal of patients experiencing urinary retention during catheterization. The characteristics of patients who undergo catheterization differ markedly from those who are capable of spontaneous voiding. In our cohort, patients with catheters exhibited a comparatively poor quality of life, reduced bladder compliance, lower BCI, and higher BOOI, as detailed in Supplementary Table 2. Furthermore, treatment goals differ between patients with and without urethral catheterization. Urinary catheterization can cause substantial discomfort and severely diminish quality of life and self-esteem. Patients with urinary catheters may focus primarily on regaining spontaneous voiding, whereas those without catheters often aim to achieve improved voiding quality— a goal that may present greater challenges. In the present study, we observed that 78% of patients who underwent urethral catheterization prior to deobstructive surgery regained spontaneous voiding. A similarly high success rate for postoperative de-catheterization was reported by Thomas et al. [15], who evaluated patients with DU and urinary retention after GLPVP. Given this success rate, coupled with the reduced risk of urinary tract infections and improvements in quality of life after catheter removal, it seems reasonable to recommend deobstructive surgery for patients experiencing urine retention due to DU, particularly when positive or equivocal BOO is present and the patient can tolerate the procedure.
The present study highlighted the usefulness of multichannel urodynamic parameters in patients with DU who underwent surgery for BOO. However, the research had several limitations. First, the study was retrospective; additionally, although its sample was large, this sample size was comparable to those of prior studies investigating interventions for DU. Second, the absence of a conservative control group means that we cannot confirm the benefits of deobstructive surgery. Nevertheless, the comparison of preoperative and postoperative outcomes sheds light on the surgical effects. Third, the lack of postoperative urodynamic studies precluded us from fully evaluating the changes in urodynamic parameters following surgery. To overcome these limitations and provide stronger evidence for future research, further prospective studies with a randomized design are necessary.
In conclusion, surgery for BOO may be advantageous in terms of IPSS, quality of life, and UFM parameters for patients with DU who also have equivocal or significant BOO. However, those with DU and an unobstructed bladder outlet face a higher risk of treatment failure. The presence of urodynamic DO and preoperative urethral catheterization were found to be associated with favorable operative outcomes. Therefore, surgery for BOO can be considered for patients with DU following urodynamic evaluation and appropriate counseling, particularly for those experiencing urinary retention.
SUPPLEMENTARY MATERIALS
Supplementary Tables 1 and 2 can be found via https://doi.org/10.5213/inj.2346252.126.
Supplementary Table 1.
Baseline demographics urodynamic parameters in patients with detrusor underactivity categorized by the type of surgery
Supplementary Table 2.
Baseline demographics and urodynamic parameters stratified by urinary catheterization
Notes
Grant/Fund Support
The work was supported by grants from the National Cheng Kung University Hospital (NCKUH-11203006). The authors would like to thank Shou-Wen Wang, Pei-Fang Lu, and Ching-Chun Lin for their contributions to this study.
Research Ethics
The Institutional Review Board (IRB) of the National Cheng Kung University Hospital approved this study (IRB number: B-ER-110-358).
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTION STATEMENT
· Conceptualization: MSC, YCO, YSC, YLK
· Data curation: MSC, YCO, YSC, KYW, YCH, CTW, YLK
· Formal analysis: MSC, YCO
· Funding acquisition: YLK
· Methodology: MSC, YCO, YSC, YLK
· Project administration: YCO, YLK
· Visualization: YLK
· Writing - original draft: MSC
· Writing - review & editing: YLK