 |
 |


- Search
| Int Neurourol J > Volume 27(4); 2023 > Article |
|
ABSTRACT
Purpose
Ischemia of the bladder can occur if neovascular formation cannot keep pace with hypoxia induced by chronic bladder outlet obstruction (BOO). The aim of this study was to examine changes in angiogenesis growth factor expression generated by chronic BOO in a rat model of underactive bladder.
Methods
Twenty female Sprague-Dawley rats aged 6 weeks were assigned to 4 groups (5 rats per group). Group 1 was the control. Group 2 underwent sham surgery. The rats in groups 3 and 4 underwent BOO and were followed up for 1 week and 8 weeks. Cystometry was carried out together with bladder tissue analysis at 1 week and 8 weeks postoperatively. Real-time polymerase chain reaction (PCR) assays were conducted to determine the expression level of angiogenesis-related growth factors. A hypoxia signaling pathway PCR array was additionally carried out.
Results
The group that underwent BOO for 8 weeks showed abnormal bladder function, with a diminished intercontraction interval, decreased maximal voiding pressure, and higher volume of residual urine (P<0.05). Hypoxia-inducible factor-1 alpha expression was elevated in this group. The expression levels of vascular endothelial growth factor (VEGF) and VEGF receptor messenger RNA (mRNA) in the BOO group were comparable to those in the control group. However, angiotensin/tie receptor mRNA expression levels increased at 1 week after BOO, but decreased at 8 weeks after BOO. In animals that underwent BOO, fewer blood vessels exhibited positive immunofluorescent staining for von Willebrand factor. Alterations were also seen in the hypoxia signaling pathway PCR array.
Conclusions
In a rat model of underactive bladder caused by surgical BOO, reduced angiopoietin expression was demonstrated. This observation might underlie visceral ischemia and fibrosis associated with the procedure. The findings of this study might offer an improved understanding of the disease processes underlying BOO and facilitate selection of the appropriate time to repair the organ in this condition.
- A rat model of bladder outlet obstruction (BOO) demonstrated reduced angiopoietin expression.
- Visceral ischemia and fibrosis are associated with BOO progression.
In aging males with benign prostatic hyperplasia (BPH), bladder outlet obstruction (BOO) frequently occurs [1,2]. Over time, BOO can lead to bladder decompensation and impaired visceral function [3]. Understanding the timeline of disease processes impacting the bladder in this scenario could aid in determining the optimal window for surgical repair.
Animal models of BOO are frequently used to explore the disease mechanisms associated with bladder problems in individuals suffering from BPH. In in vivo experiments, BOO can induce early hypertrophy of the detrusor muscle and increase intravesical pressure to maintain steady urine flow [1-3]. This process can compromise the blood supply to the detrusor muscle, leading to ischemia, which plays a significant role in abnormal detrusor function. As a consequence, metabolism may shift towards anaerobic mechanisms [4,5].
The transcription factor hypoxia-inducible factor 1-alpha (HIF1-α) is a crucial mediator in mammalian cells, becoming active only under conditions of cellular hypoxia [6,7]. As an oxygen-dependent transcriptional activator, it has the ability to activate genes involved in glucose transport and metabolism. It is also responsible for amplifying the expression of genes known to contribute to cell survival and programmed cell death [8]. In particular, the upregulation of HIF1-α can stimulate the expression of proangiogenic gene products, including vascular endothelial growth factor (VEGF) [9].
BOO can lead to compensatory changes within the bladder. These changes may provide a deeper understanding of the disease processes underlying the condition, thereby assisting in determining the optimal timing for bladder repair in patients with BOO. The expression of HIF1-α, VEGF/VEGF receptor, and angiopoietin/angiopoietin receptor might serve as potential markers of tissue hypoxia and visceral adaptation. The aim of the current study was to measure the mRNA levels of these factors in a rat BOO model, in order to investigate the bladder’s initial response to injury caused by BOO.
All protocols in this study adhered to the National Institute of Health Guide for the Care and Use of Laboratory Animals. The study received approval from the Institutional Animal Care and Use Committee of the clinical facility. The BOO model used in this study was developed by replicating the study protocol previously conducted by the authors [10,11].
Twenty female Sprague-Dawley rats, aged 6 weeks, were divided into 4 groups, with each group containing 5 rats. Group 1 (n=5) served as the control, while group 2 (n=5) underwent sham surgery. Groups 3 (n=5) and 4 (n=5) underwent BOO surgery and were monitored for 1 week and 8 weeks, respectively. BOO surgery was performed on the relevant rats under isoflurane (BK Pharm, Goyang, Korea) anesthesia. A skin incision was made in the lower abdomen, followed by urethral dissection. Subsequently, 4-0 silk sutures were used to encircle the urethra, with a 1-mm external diameter metal rod placed outside the lumen. Once the sutures were placed, the rod was removed and the abdominal wound was closed. For infection prophylaxis, cephalosporin (Flomoxef, BK Pharm, Goyang, Korea, 10 mg/kg per day) was administered interperitoneally.
Eight weeks after BOO surgery, the voiding response was evaluated in all rats by inserting a PE-50 catheter into the bladder. After the administration of an isoflurane anesthetic, a midline abdominal incision was made to expose the bladder. A collar was formed by warming the bladder end of the catheter, which was then positioned in the bladder via a tiny incision in the bladder dome and held in place by a suture. The opposing catheter end was threaded through the subcutaneous tissue to exit the skin. The wound was closed by suturing muscular and dermal layers. Anesthesia was then terminated.
The rats were housed in a restraining cage for 6 hours, which included a 2-hour recovery period following the surgical anesthesia. The dimensions of the cage were designed to allow the rats to crouch comfortably, but not to turn around. Once the rats had fully recovered from the isoflurane anesthesia, a pump was connected to the bladder catheter via a T-stopcock. This setup facilitated the continuous infusion of physiological saline, maintained at room temperature, into the bladder at a rate of 0.04 mL/min. The pump was also linked to a pressure transducer. The saline infusion triggered multiple voiding responses in the rats. The urination reflexes induced by volume loading were studied in the restrained rats. The parameters that were recorded included the intravesical pressure necessary for micturition, the pressure threshold (PT), the maximal voiding pressure (MVP), and the intercontraction interval (ICI). The ICI was defined as the time elapsed between voiding episodes or reflex bladder contractions.
After cystometry, the rats were euthanized via an intracardiac infusion of 100 mL of cold saline and 100 mL of 4% paraformaldehyde in phosphate-buffered saline, while under anesthesia. The bladder was subsequently extracted from each rodent and preserved in 4% paraformaldehyde for 48 hours. The viscera were then cryoprotected using 30% sucrose for 72 hours. Subsequently, a cryostat (Leica CM 1900, Leica, Wetzlar, Germany) was employed to cut sections of 10-μm thickness. These sections were then subjected to fluorescent staining and immunofluorescence processing. The samples were examined using an Olympus laser confocal fluorescence microscope.
The samples were subjected to immunostaining to detect the presence of von Willebrand factor (vWF) (1:200, Abcam, Cambridge, UK). Antigens were extracted following a 10-minute warming period with 9mM sodium citrate at a pH of 5. To inhibit intrinsic peroxidase activity, a peroxidase-blocking reagent (Dako, Carpinteria, CA, USA) was utilized. Free-floating tissue sections were incubated overnight at 4°C using a mixed primary antibody solution for vWF. Subsequently, Alexa Fluor 488-conjugated anti-mouse IgG (1:200, Molecular Probe, Eugene, OR, USA) and Alexa Fluor 594-conjugated anti-rabbit IgG (1:200, Molecular Probe) were added, followed by an additional 60-minute incubation at room temperature. A negative control specimen was prepared in the same manner, but without the inclusion of primary antibodies. The stained samples were examined using an Olympus laser confocal fluorescence microscope. Quantitative analysis of the histological examinations was conducted using an image analyzer system (National Institutes of Health Image J 1.34, http://rsbweb.nih.gov/ij/).
As stated above, the rodents were sacrificed after cystometry was completed. The bodies of the bladders were removed and dissected away from any attached soft tissues prior to weighing. They were placed directly into a freezer in liquid nitrogen until additional biochemical and molecular biological assessments were required.
The Trizol reagent (Invitrogen, Carlsbad, CA, USA) was used to extract total DNAs from cells and samples. Real-time polymerase chain reactions (PCRs) were carried out. The threshold cycle value was the basis for assaying relative gene expression. Normalization was performed against β-actin as a housekeeping gene. Data averaged over 3 experiments are presented. The PCR procedure comprised the following stages: 95°C for 10 seconds, and 40 cycles of 95°C for 5 seconds and 60°C for 30 seconds. Lastly, melting curve analysis over 60°C–95°C was carried out.
To isolate and extract total RNA, an RNA extraction kit (RNeasy Mini Kit, QIAGEN, Hilden, Germany) was used following the manufacturer’s instructions. The extracted RNA solution was treated with RNase-free DNase (QIAGEN, Hilden, Germany) to ensure there was no DNA contamination. Using an RT2 First Strand Kit (QIAGEN) and 2 μg of total RNA, the initial cDNA strand was synthesized in accordance with the manufacturer’s recommendations. This was then combined with RT2 quantitative PCR master mixes. Small quantities of this mixture were placed in a 96-Well RT2 Profiler PCR Array for rat hypoxia (QIAGEN). This array included SYBR green-optimized primer assays for a carefully selected panel of genes relevant to the pathway, consisting of 84 genes associated with the hypoxic response and 12 genes serving as a reference for the quality of loading and cDNA. The real-time PCR assay was conducted by heating the plate for 10 minutes at 95°C, followed by 40 cycles of 15 seconds at 95°C and 60 seconds at 60°C. Quality assurance was provided by genomic DNA, reverse transcription, and positive PCR controls. β-actin served as the housekeeping gene. Any changes in gene expression were represented as a factor of increase or decrease, with a cutoff value of changes over a factor of 2 defining upregulated or downregulated expression. The primers used for real-time PCR for hypoxia are listed in Table 1.
The mean body mass of the rats in the sham surgical group and groups receiving BOO were equivalent (266±3.3 g and 235±7.1 g, respectively). The rats that underwent sham surgery had a significantly lower bladder weight (86.9±8.5 mg vs. 242.2±7.8 mg) than those that underwent a BOO procedure (242.2±7.9 mg) (P<0.05) (Fig. 1).
In rats that underwent BOO, the ICI was considerably higher (1,384±214 seconds) than in the sham surgical cohort (390±58 seconds, P<0.05). The PT values for the 2 groups were comparable (7.8±0.7 cm H2O in the sham surgical group and 8.0±0.8 cm H2O in the BOO cohort). The BOO group showed a lower MVP than the sham surgery group (23.7±4.1 cm H2O vs. 34.7±7.4 cm H2O) with elevated RU (6.4±1.5 mL vs. 0.1±0.08 mL) (Fig. 2).
Relative to the control group, HIF-1α mRNA expression levels were similar in rats that underwent BOO at week 1, but increased at 8 weeks following the BOO procedure (P<0.05). VEGFA and VEGFR2 mRNA expression levels at 1 week and 8 weeks following BOO were similar to those in the control group.
Compared with rats in the sham surgery group, the group at 1 week after BOO demonstrated higher levels of angiopoietin-1 (Ang-1), Ang-2, Ang-4, and Tie2 mRNA expression (Fig. 3). However, these levels were diminished at 8 weeks after BOO (P<0.05).
Fewer vWF-positive blood vessel configurations were identified on immunofluorescence staining in rats that underwent BOO (P<0.05) (Fig. 4).
Hif3a (-39.6) and Per1 (-5.1) were among the HIF and cotranscription factors. Additional HIF interactors included cyclin-dependent kinase inhibitor 2A (Cdkn2a, 11.0). Early growth response 1 (Erg1, 4.2), matrix metalloproteinase 9 (Mmp9, 74.7), serpin peptidase inhibitor, clade E, member 1 (Serpine1, 11.0), lysyl oxidase (LOX, 6.0), and heme oxygenase 1 (Hmox1, 6.1) were related to angiogenesis (Fig. 5).
BOO can lead to mural thickening of the bladder and hypertrophy, which can improve bladder stability and facilitates adaptation to the requirement to void against an increase in resistance in the urethra caused by the obstruction [12,13]. Mural thickening creates a cycle of ischemia and reperfusion during the urination cycle [14,15]. Hypoxia in the bladder has been observed in the smooth detrusor muscle and bladder subserosa [16]. This oxygen deficit is associated with impaired contractile function and metabolic abnormalities in the smooth muscle.
In this study, BOO significantly affected the mass of the bladder (Fig. 1). BOO compromises mural perfusion in the bladder. Bladder contractions can result in reduced oxygen tension, which is then reversed after the bladder is emptied [14,17]. The viscera can adapt if BOO persists for only a short period. However, in the context of ongoing BOO, repeated episodes of hypoxia can lead to progressive functional impairment and bladder decompensation.
It has been established that a decrease in detrusor perfusion, observed immediately following BOO, correlates with the degree of bladder decompensation [17]. This decompensation occurs as the detrusor muscle undergoes repetitive phases of ischemia and reperfusion, leading to the production of reactive free radicals. Furthermore, the activation of specific phospholipase and protease enzymes can contribute to the membrane damage observed at both cellular and subcellular levels [18].
In the present study, we observed increases in ICI and RU, and a decrease in MVP (Fig. 2). Rapid alterations in the bladder’s configuration and functionality are initiated following the onset of BOO. Initially, the MVP increases to maintain a steady urine flow, while the ICI decreases [1-3]. Significant bladder decompensation was induced following BOO, resulting in the parameter changes as described. In a system where BOO exists, the process of filling and emptying the bladder can trigger a cycle of ischemia and reperfusion within the viscera. This cycle can rapidly alter the oxygenation status of a tissue [19]. For hypoxia to be rectified, angiogenesis is essential. The term angiogenesis refers to the formation of new arterial and venous vessels. These may originate from pre-existing vasculature (for instance, through the creation of de novo vessels from current vascular conduits or by the division of these conduits), or from the formation of neovascular vessels as a result of sprouting angiogenesis [19,20].
Earlier studies have documented a close link between low oxygen levels and HIF-1α [21-23]. In mammalian cells, the transcription factor HIF-1α is responsible for the hypoxia response. This mediator is only functional under conditions of cellular hypoxia [6,7]. As an oxygen-dependent transcriptional activator, HIF-1α can enhance the activity of genes associated with glucose transport and metabolism. It can also trigger the upregulation of a gene that aids in maintaining cellular viability [8]. The HIF-1α transcription factor is the primary initiator of the hypoxia signaling pathway when oxygen availability is reduced. A variety of biological activities, such as angiogenesis, hematopoiesis, and the maintenance of vascular tone to ensure the delivery of blood and oxygen to tissues, are regulated by target genes that respond to low oxygen levels. In the rat model used in this study, BOO resulted in a minor change in HIF-1α levels after 1 week. However, after 8 weeks, a significant increase in HIF-1α levels was observed. This suggests that short-term BOO (e.g., 1 week) does not lead to bladder hypoxia, while long-term BOO (e.g., 8 weeks) does have hypoxic effects (Fig. 3).
It has been observed that alongside HIF-1α in BOO, VEGF levels also increase [24,25]. VEGF, which is an angiogenic factor and a diffusible mitogen specific to endothelial cells, increases the permeability of the vasculature, leading to substantial neovascular formation.
VEGFA is a prominent member of the VEGF family. Endothelial cells (ECs) are the only cells that express VEGFR2. This factor is potentially critical for the differentiation of ECs and the formation of blood vessels [24,25]. The modest alteration in HIF-1α levels observed in this study at week 1 failed to cause an increase in VEGF. Interestingly, no elevation in VEGF levels was seen at week 8 despite increased HIF-1α levels (Fig. 3). VEGFR2 expression remained relatively constant in rats that underwent BOO, both at 1 week and 8 weeks after BOO. The duration of BOO was sufficient to imply that these results indicated a failure of VEGF and VEGFR to respond to the increase in HIF-1α.
Angiogenesis is controlled at specific points by Ang-1 and VEGF. The latter promotes the sprouting and development of vascular conduits, whereas the former contributes to the maturation and remodeling of blood vessels [26]. VEGF influences the formation of new blood vessels, but the conduits it creates are structurally immature. This is evident in their lack of uniform appearance, tortuosity, dead ends, and disordered arrangement of venules, arterioles, and capillaries. Functionally, these conduits are also deficient, as they leak blood cells, which can lead to increased interstitial pressure.
ECs are responsible for establishing the vascular system, working in conjunction with auxiliary mural cells such as small capillary pericytes and smooth muscle cells from larger caliber vessels. These cell types work in close collaboration during the processes of neovasculature sprouting, cell migration and replication, and blood vessel maturation. They aid in the formation of new vessels that interconnect to form a well-branched network of conduits. This network facilitates the transport of fluids, nutrients, gases, hormones, and cells within the circulatory system throughout the body of a vertebrate organism. The remodeling and maturation of vessels, as well as the recruitment of mural cells during vasculature homeostasis in adults, have been shown to rely on the tyrosine kinase with immunoglobulin and EGF homology domains (Tie), angiopoietin receptor system [27]. In pericytes and smooth muscle cells, low oxygen levels and VEGF have been found to increase the expression of Ang-1. This, in conjunction with VEGF expression, can facilitate the development of well-differentiated vasculature. In mice expressing VEGFA alone, the Ang/Tie system was observed to counteract vessel leakage and permeability. The signaling function of the Ang/Tie system appears to act as a supplementary mechanism in the presence of VEGF and VEGFR.
Ang-2 is considered to have only partial agonistic activity due to its lower affinity for Tie2 compared to Ang-1. The role of Ang-3 and Ang-4 in neovascular formation related to disease has not yet been thoroughly investigated [28].
The current data demonstrated that, compared to rats that underwent sham surgery, rats 1-week post-BOO exhibited elevated levels of Ang-1/Tie and VEGF, as well as Ang-1, Ang-2, and Ang-4. The expression levels of these factors decreased in rats after 8 weeks of BOO (P<0.05) (Fig. 3). Tie2 followed a similar pattern (P<0.05) (Fig. 3). Survival under the low bladder oxygen levels induced by BOO necessitates the stimulation of angiogenesis to increase VEGF/VEGFR and Ang/Tie levels. There was no immediate increase in the former. However, HIF-1α expression was enhanced, and a decrease in angiopoietins along with their receptors was observed 8 weeks after BOO.
When the bladder is chronically underactive, it exhibits decompensation. Hypoxia can trigger an inappropriate reaction. Rather than VEGF/VEGFR promoting angiogenesis, Ang/Tie responds to the low oxygen tension to ensure survival. These findings suggest that bladder angiogenesis may be promoted to compensate for the new metabolic condition that arises 1 week after BOO. However, this response was diminished at 8 weeks after BOO. Hypoxia has been observed in the smooth detrusor muscle and the bladder subserosa [16]. The BOO cohort exhibited fewer vascular conduits and a lower vessel density compared to rats that underwent sham surgery or controls, as evidenced by vWF immunofluorescence staining (Fig. 4). Low oxygen tension resulting from the surgical procedure was noted.
The 96-Well RT2 Profiler PCR Array for rat hypoxia (QIAGEN) includes SYBR green-optimized primer assays for a carefully selected panel of genes pertinent to the pathway. This array covers 84 genes linked to the hypoxic response. In our recent study, we analyzed bladder samples taken from rats 8 weeks after BOO. We found that the expression of HIF3a, a gene known to negatively mediate gene expression under low oxygen conditions, was downregulated by a factor of 39.6 (Fig. 5). This suggests that Hif3a may have a positive influence on gene expression in hypoxic conditions. In the same group of rats, we observed a downregulation of Per1, which is associated with HIF and cotranscription factors, by a factor of 5.1 in bladder samples. We also noted an upregulation of Cdkn2a, a secondary HIF1 interactor, by a factor of 11.0. Furthermore, the genes erg1, Serpine 1, and Hmox1 were upregulated by factors of 4.2, 11.0, and 6.1, respectively. This specific gene expression pattern could potentially explain the molecular disease processes observed in a decompensated bladder with BOO, which is associated with the activation of the HIF-1 pathway.
Many disease mechanisms are considered to result from low oxygen tension, such as the deposition of extracellular matrices and changes in smooth muscle function [29]. LOX, an extracellular enzyme, can facilitate covalent crosslinking between type I and type III collagen fibers, thereby enhancing the stiffness and stability of extracellular collagen [30]. Upregulation of LOX by a factor of 6.0 was observed in the bladders of rats at 8 weeks after BOO. In angiogenesis and wound reparation, degradation of the extracellular membrane is caused by matrix metalloproteinases (MMPs) [31]. Upregulation of Mmp9 by a factor of 74.7 was seen in the current work, suggesting a positive influence of Mmp9 on angiogenesis within the bladder at 8 weeks after BOO. These results established that sprouting of the endothelium, enhanced permeability of the vasculature, tissue MMP expression, and ultimately, matrix digestion, are necessary for cellular migration. This research provides evidence regarding changes in the pathways of hypoxia-related genes in response to BOO.
NOTES
Grant/Fund Support
This research was supported by a grant from Soonchunhyang University Research Fund and the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2021R1A2C1004163).
Research Ethics
The Institutional Animal Care and Use Committee of the Soonchunhyang University Hospital granted approval for the procedures (No. 2019-4), which were carried out in conformance to the National Institute of Health Guide for the Care and Use of Laboratory Animals.
AUTHOR CONTRIBUTION STATEMENT
· Conceptualization: HJL, YSS
· Data curation: JHK
· Formal analysis: JHK, HJL
· Funding acquisition: YSS
· Methodology: HJY, HJL, YSS
· Project administration: JHK, HJY
· Visualization: HJY
· Writing - original draft: JHK, HJY, HJL, YSS
· Writing - review & editing: JHK, HJY, HJL, YSS
REFERENCES
1. Brent L, Stephens FD. The response of smooth muscle cells in the rabbit urinary bladder to outflow obstruction. Invest Urol 1975;12:494-502. PMID: 1120643

2. Saito M, Wein AJ, Levin RM. Effect of partial outlet obstruction on contractility: comparison between severe and mild obstruction. Neurourol Urodyn 1993;12:573-83. PMID: 7508779


3. Mostwin JL, Karim OM, van Koeveringe G, Brooks EL. The guinea pig as a model of gradual urethral obstruction. J Urol 1991;145:854-8. 
4. Koritsiadis G, Stravodimos K, Koutalellis G, Agrogiannis G, Koritsiadis S, Lazaris A, et al. Immunohistochemical estimation of hypoxia in human obstructed bladder and correlation with clinical variables. BJU Int 2008;102:328-32. PMID: 18384635


5. Saito M, Longhurst PA, Tammela TL, Wein AJ, Levin RM. Effects of partial outlet obstruction of the rat urinary bladder on micturition characteristics, DNA synthesis and the contractile response to field stimulation and pharmacological agents. J Urol 1993;150:1045-51. PMID: 8102184


6. Semenza GL. HIF-1 and mechanisms of hypoxia sensing. Curr Opin Cell Biol 2001;13:167-71. PMID: 11248550


7. Huang LE, Gu J, Schau M, Bunn HF. Regulation of hypoxia-inducible factor 1alpha is mediated by an O2-dependent degradation domain via the ubiquitin-proteasome pathway. Proc Natl Acad Sci U S A 1998;95:7987-92. PMID: 9653127


8. Liu P, Hock CE, Nagele R, Wong PY. Formation of nitric oxide, superoxide, and peroxynitrite in myocardial ischemia-reperfusion injury in rats. Am J Physiol 1997;272:H2327-36. 
9. Rivard A, Berthou-Soulie L, Principe N, Kearney M, Curry C, Branellec D, et al. Age-dependent defect in vascular endothelial growth factor expression is associated with reduced hypoxia-inducible factor 1 activity. J Biol Chem 2000;275:29643-7. 
10. Lee HJ, Won JH, Doo SH, Kim JH, Song KY, Lee SJ, et al. Inhibition of collagen deposit in obstructed rat bladder outlet by transplantation of superparamagnetic iron oxide-labeled human mesenchymal stem cells as monitored by molecular magnetic resonance imaging (MRI). Cell Transplant 2012;21:959-70. PMID: 22449414



11. Kim JH, Yang HJ, Choi SS, Kim SU, Lee HJ, Song YS. Improved bladder contractility after transplantation of human mesenchymal stem cells overexpressing hepatocyte growth factor into underactive bladder from bladder outlet obstruction models of rats. PLoS One 2021;16:e0261402. PMID: 34936660



12. Kato K, Monson FC, Longhurst PA, Wein AJ, Haugaard N, Levin RM. The functional effects of long-term outlet obstruction on the rabbit urinary bladder. J Urol 1990;143:600-6. PMID: 1968106


13. Levin RM, Longhurst PA, Barasha B, McGuire EJ, Elbadawi A, Wein AJ. Studies on experimental bladder outlet obstruction in the cat: long-term functional effects. J Urol 1992;148:939-43. PMID: 1512863


14. Greenland JE, Hvistendahl JJ, Andersen H, Jörgensen TM, Mc-Murray G, Cortina-Borja M, et al. The effect of bladder outlet obstruction on tissue oxygen tension and blood flow in the pig bladder. BJU Int 2000;85:1109-14. PMID: 10848706


15. Greenland JE, Brading AF. The effect of bladder outflow obstruction on detrusor blood flow changes during the voiding cycle in conscious pigs. J Urol 2001;165:245-8. PMID: 11125418


16. Levin RM, Yu HJ, Kim KB, Longhurst PA, Wein AJ, Damaser MS. Etiology of bladder dysfunction secondary to partial outlet obstruction. Calcium disregulation in bladder power generation and the ability to perform work. Scand J Urol Nephrol Suppl 1997;184:43-50. PMID: 9165622

17. Schröder A, Chichester P, Kogan BA, Longhurst PA, Lieb J, Das AK, et al. Effect of chronic bladder outlet obstruction on blood flow of the rabbit bladder. J Urol 2001;165:640-6. PMID: 11176451


18. Gosling JA, Kung LS, Dixon JS, Horan P, Whitbeck C, Levin RM. Correlation between the structure and function of the rabbit urinary bladder following partial outlet obstruction. J Urol 2000;163:1349-56. PMID: 10737542


19. Zhao Y, Levin SS, Wein AJ, Levin RM. Correlation of ischemia/reperfusion or partial outlet obstruction-induced spectrin proteolysis by calpain with contractile dysfunction in rabbit bladder. Urology 1997;49:293-300. PMID: 9037302


20. Adams RH, Alitalo K. Molecular regulation of angiogenesis and lymphangiogenesis. Nat Rev Mol Cell Biol 2007;8:464-78. PMID: 17522591



21. Hoskin PJ, Sibtain A, Daley FM, Wilson GD. GLUT1 and CAIX as intrinsic markers of hypoxia in bladder cancer: relationship with vascularity and proliferation as predictors of outcome of ARCON. Br J Cancer 2003;89:1290-7. PMID: 14520462




22. Lee JW, Bae SH, Jeong JW, Kim SH, Kim KW. Hypoxia-inducible factor (HIF-1)alpha: its protein stability and biological functions. Exp Mol Med 2004;36:1-12. PMID: 15031665



23. Hoppeler H, Vogt M. Muscle tissue adaptations to hypoxia. J Exp Biol 2001;204:3133-9. PMID: 11581327



24. Millauer B, Wizigmann-Voos S, Schnürch H, Martinez R, Møller NP, Risau W, et al. High affinity VEGF binding and developmental expression suggest Flk-1 as a major regulator of vasculogenesis and angiogenesis. Cell 1993;72:835-46. PMID: 7681362


25. Quinn TP, Peters KG, De Vries C, Ferrara N, Williams LT. Fetal liver kinase 1 is a receptor for vascular endothelial growth factor and is selectively expressed in vascular endothelium. Proc Natl Acad Sci U S A 1993;90:7533-7. PMID: 8356051



26. Thurston G, Suri C, Smith K, McClain J, Sato TN, Yancopoulos GD, et al. Leakage-resistant blood vessels in mice transgenically overexpressing angiopoietin-1. Science 1999;286:2511-4. PMID: 10617467


27. Thurston G. Role of angiopoietins and Tie receptor tyrosine kinases in angiogenesis and lymphangiogenesis. Cell Tissue Res 2003;314:61-8. PMID: 12915980



28. Yuan HT, Khankin EV, Karumanchi SA, Parikh SM. Angiopoietin 2 is a partial agonist/antagonist of Tie2 signaling in the endothelium. Mol Cell Biol 2009;29:2011-22. PMID: 19223473




29. Higgins DF, Kimura K, Bernhardt WM, Shrimanker N, Akai Y, Hohenstein B, et al. Hypoxia promotes fibrogenesis in vivo via HIF-1 stimulation of epithelial-to-mesenchymal transition. J Clin Invest 2007;117:3810-20. PMID: 18037992



30. Aitken KJ, Bägli DJ. The bladder extracellular matrix. Part I: architecture, development and disease. Nat Rev Urol 2009;6:596-611. PMID: 19890339



31. Page-McCaw A, Ewald AJ, Werb Z. Matrix metalloproteinases and the regulation of tissue remodelling. Nat Rev Mol Cell Biol 2007;8:221-33. PMID: 17318226




Fig. 1.
Changes in body and bladder weight 8 weeks after BOO surgery. There was no significant difference in body weight between groups. The group with BOO showed greater bladder weight than the sham operation group. Sham, sham operation; BOO, bladder outlet obstruction. *P<0.05.
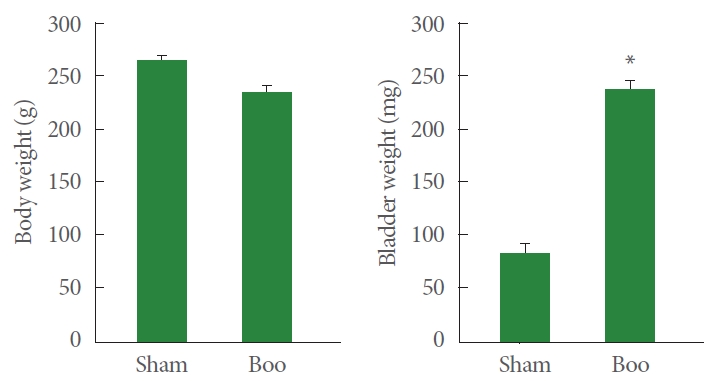
Fig. 2.
Recovery of cystometric parameters 8 weeks after BOO surgery. The BOO group showed higher ICI and RU than the sham surgery group. The BOO group showed lower MVP than the sham surgery group. Sham, sham operation; BOO, bladder outlet obstruction; BOO+hMSCs, human mesenchymal stem cell injection at 2 weeks after bladder outlet obstruction; ICI, intercontraction interval; MVP, maximal voiding pressure; PT, pressure threshold; RU, residual urine volume. *P<0.05.
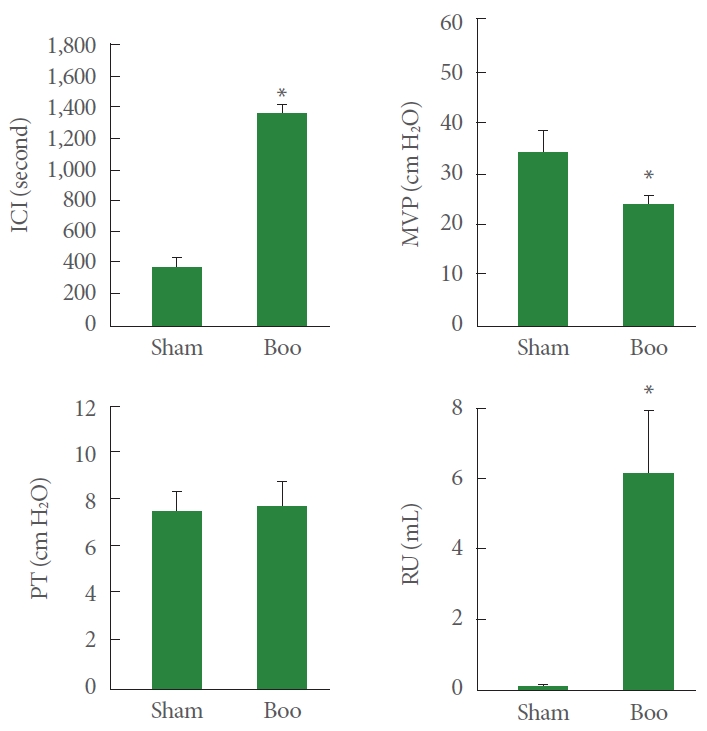
Fig. 3.
Messenger RNA (mRNA) expression in the bladder of the BOO group. mRNA expression of HIF-1α at 8 weeks after BOO was higher than that in the control group at 8 weeks after BOO surgery (#P<0.05). mRNA expression levels of angiopoietin-1 (Ang-1), Ang-2, and Ang-4 were increased at 1 week after BOO (*P<0.05) but decreased at 8 weeks after BOO (#P<0.05). mRNA expression of Tie2 was increased at 1 week after BOO (*P<0.05) but decreased at 8 weeks after BOO (#P<0.05). Sham, sham operation; BOO, bladder outlet obstruction; HIF-1α, hypoxia-inducible factor-1 alpha; VEGFA, vascular endothelial growth factor A; VEGFR, vascular endothelial growth factor receptor; Tie, tyrosine kinase with immunoglobulin and EGF homology domains, angiopoietin receptor.

Fig. 4.
Immunofluorescence staining of bladder tissues. Staining with vWF demonstrates fewer vWF-positive blood vessel structures in the group that underwent BOO. DAPI, 4´-6-diamidino-2-phenylindole; vWF, von Willebrand factor; Sham, sham operation; BOO, bladder outlet obstruction. *P<0.05.

Fig. 5.
Polymerase chain reaction array of hypoxia signaling pathways in the bladders of BOO rats. HIF and cotranscription factors including Hif3a (-39.6) and Per1 (-5.1), other HIF1 interactors including Cdkn2a (11.0), and angiogenesis-related factors including Erg1 (4.2), Mmp9 (74.7), Serpine1 (11.0), Lox (6.0), and Hmox1 (6.1) were compared with those in the sham operation group. Changes were confirmed by heat mapping. HIF, hypoxia-inducible factor.
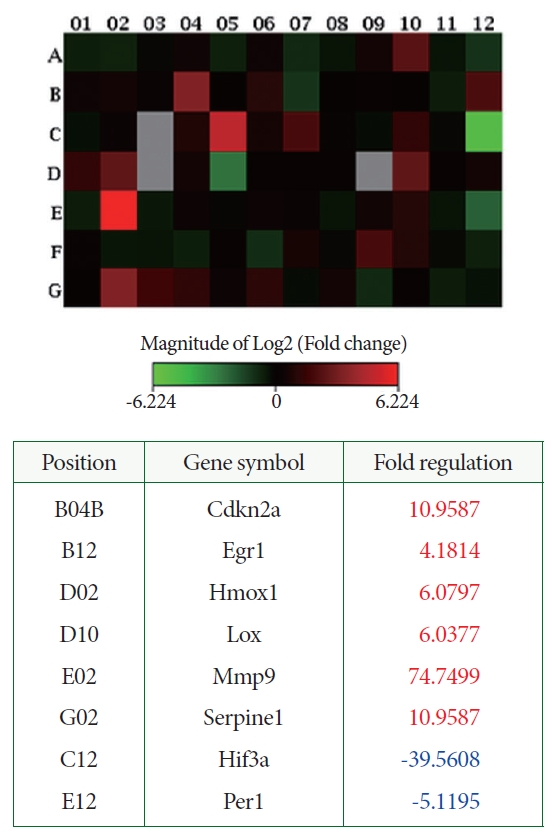
Table 1.
Primer used for real-time polymerase chain reaction





