 |
 |


- Search
| Int Neurourol J > Volume 27(2); 2023 > Article |
|
ABSTRACT
Purpose
This is the first report to compare 3-dimensional computed tomography (3D-CT) images between pediatric patients with enuresis and children without lower urinary tract symptoms who underwent pelvic CT for other reasons.
Methods
Forty-seven children (33 boys and 14 girls) with primary enuresis underwent 3D-CT of sacrococcygeal bones. The control group consisted of 138 children (78 boys and 60 girls) who underwent pelvic CT for other reasons. First, we determined the presence or absence of unfused sacral arches at the L4-S3 levels in both cohorts. Subsequently, we compared the fusion of sacral arches in age- and sex-matched children from these 2 groups.
Results
Dysplastic sacral arches, characterized by lack of fusion at 1 or more levels of the S1–3 arches, were observed in nearly all patients in the enuresis group. In the control group (n=138), 54 of 79 children over 10 years old (68%) exhibited fused sacral arches at 3 S1–3 levels. All 11 control children under 4 years old displayed at least 2 unfused sacral arches at the S1–3 levels. In a comparative study of age- and sex-matched patients with enuresis and control children aged 5 to 13 years (n=32 for each group, with 21 boys and 11 girls; mean age, 8.0±2.2 years [range, 5–13 years]), only 1 patient (3%) in the enuresis group exhibited fusion of all S1–3 arches. In contrast, 20 of 32 control group participants (63%) had 3 fused sacral arches (P<0.0001).
Conclusions
Sacral vertebral arches typically fuse by the age of 10 years. However, in this study, children with enuresis exhibited a significantly elevated prevalence of unfused sacral arches, suggesting that dysplastic development of sacral vertebral arches may play a pathological role in enuresis.
Enuresis is defined as the voluntary or involuntary wetting of clothes or bedding with urine for at least 3 consecutive months in children older than 5 years [1]. This condition can negatively impact a child’s psychosocial growth, potentially hindering the development of self-confidence and the ability to socialize [2]. Previous studies have reported that deformities of the lumbosacral vertebral arches, commonly identified as spina bifida occulta, are occasionally observed in cases of persistent enuresis [3-6]. Additionally, research indicates that the response rate to behavioral and pharmacological treatments is lower in children with enuresis and spina bifida occulta than in those without [7,8]. However, those studies primarily involved the use of conventional plain pelvic x-ray films to detect the presence or absence of fusion in the lumbar and/or sacral spinous processes. Most such studies revealed incomplete vertebral fusion at the L4–5 lumbar or S1 sacral spinal levels, while the major neural pathways controlling lower urinary tract function in humans actually emerge from the S2–3 spinal levels [9].
Three-dimensional computed tomography (3D-CT) has recently become a common radiographic modality in the field of bone and joint diseases, encompassing complicated fractures and even tumors [10]. Consequently, the present study employed 3D-CT techniques, as opposed to plain x-ray films, for the first time to compare 3D-CT images of the fusion status of vertebral arches at the L4 to S3 spinal levels in 2 cohorts. These were (1) pediatric cases with enuresis and (2) children without lower urinary tract symptoms who underwent pelvic CT for other reasons. Our objective was to evaluate the age-dependent fusion status of the sacral vertebral arches in a control group of children, as well as the difference in the prevalence of dysplastic development of sacral vertebral arches between the 2 cohorts.
Between January 2019 and December 2019, 47 children visited our outpatient clinic for primary nocturnal enuresis and underwent 3D-CT of the sacrococcygeal bone (33 boys and 14 girls; mean age, 7.9±2.0 years; range, 5–13 years). The control group consisted of 138 children without enuresis (78 boys and 60 girls; mean age, 10.7±4.4 years; range, 3 months to 18 years) who underwent conventional pelvic CT. The reasons for hospital visits among the children in the control group included abdominal pain (27.5%), fever (18.1%), vomiting and nausea (15.9%), diarrhea (13.0%), trauma (9.4%), back pain (8.7%), hematemesis (3.6%), hematuria (2.2%), and others. These children were asked about lower urinary tract symptoms and/or episodes of nocturnal enuresis during interviews in the pediatric outpatient clinic or the Emergency Department. Children who had lower urinary tract symptoms, including nocturnal enuresis, were then excluded from the control group of this study.
Pelvic CT images from the control group were reconstructed into 3D-CT images and then compared with the 3D-CT images from the enuresis group. After an initial comparison between the 2 groups with all participants included, 32 age- and sexmatched pairs were selected, each consisting of 1 control child and 1 child with enuresis (n=32 in total, with 21 boys and 11 girls in each group; mean age, 8.0±2.2 years; range, 5–13 years). This selection was made to avoid potential sex- or age-related statistical biases, and the pairs were compared regarding the presence or absence of fusion in the dorsal sacral arches (S1–3) and lower lumbar arches (L4–5). For imaging analyses, we focused on the deformity of vertebral arches at the sacral level, where autonomic nerves to the lower urinary tract emerge [9]. All values are presented as means±standard deviations. Statistical analysis was performed using the Student t-test, and a P-value of <0.05 was considered to indicate statistical significance.
A comparison between plain x-ray and 3D-CT images is shown in Fig. 1. On the plain x-ray film, assessing the fusion status of the sacral vertebral arches is challenging. In contrast, 3D-CT images clearly reveal the vertebral arches, allowing for evaluation of whether these arches are bilaterally fused at each level of the S1–3 sacral bone.
In the initial assessment of all participants, dysplastic sacral vertebral arches, characterized by lack of fusion at one or more of the S1–3 levels, were observed in every case within the enuresis group (n=47) (Fig. 1). In the control group (n=138), among the 79 children who were over 10 years old, 54 cases (68%) exhibited fused sacral arches at all S1–3 levels (Fig. 2), while the remaining 25 control children over 10 years old (32%) had one or more unfused sacral arches at those levels. Eleven control children were under 4 years old, all of whom displayed at least 2 unfused sacral arches at the S1–3 levels. These results from the control group suggest that the sacral vertebral arches at the S1–3 levels remain unfused during infancy but become fused by age 10 in most children. In contrast, in the enuresis group, only 2% of cases demonstrated fusion of all 3 sacral arches; in other words, 98% of children with enuresis had an unfused sacrum (Table 1). In contrast, the L4–5 lower lumbar arches showed high rates of fusion in both groups, suggesting that the fusion rate of lumber arches was not significantly associated with the incidence of nocturnal enuresis (Table 1).
The initial analysis revealed an age-dependent maturation process of sacral arch fusion within the control group. To avoid age-related bias, a subsequent statistical comparison study was conducted using age-matched enuresis and control groups of children aged 5 to 13 years (n=32 each). Among the 32 children with enuresis, only 1 (3%) exhibited fusion of all 3 sacral arches at the S1–3 levels. In contrast, 20 of 32 children (63%) in the control group had fused arches at all S1–3 levels (P<0.0001; Student t-test) (Table 2).
Nocturnal enuresis is a common pediatric condition, affecting approximately 10%–15% of 5-year-old children [11,12]. An annual spontaneous remission rate of 15% is often cited [13]. Since spontaneous remission is common, delayed maturation of anatomical structures is a plausible cause of nocturnal enuresis. However, until recently, anatomic abnormalities of the sacral vertebrae had not been thoroughly examined in children with nocturnal enuresis. To our knowledge, the present study is the first to report a delay in the anatomical maturation of sacral vertebral arches that may be involved in nocturnal enuresis in infants, using the 3D-CT imaging technique. We hypothesize that this delay in anatomical maturation could partially explain the etiology of nocturnal enuresis, as spontaneous remission is common in both nocturnal enuresis and unfused sacral arches. This study indicated that, in nocturnal enuresis, the sacral vertebral arches do not properly close during childhood. These findings align with previous studies demonstrating an association between spina bifida occulta, evident as incomplete vertebral fusion at the lumbosacral spinal levels, and nocturnal enuresis [3-8]. However, those previous studies utilized conventional plain pelvic x-ray films, and they primarily showed unfused vertebral arches at the L4 and L5 spinal levels. In contrast, the present study involved 3D-CT imaging and revealed that the L4–5 spinal arches are similarly fused in both control children and those with enuresis, whereas unfused S1–3 spinal arches are highly prevalent in enuresis versus control children. Ultimately, unfused sacral arches at 1 or more S1–3 levels were observed at a high rate (98%) in the enuresis group (Table 1). These results suggest that the 3D-CT technique, which allows for clearer observation of the posterior side of the sacrum compared to plain x-ray films, is useful for detecting dysplastic changes in the S1–3 vertebral arches (Fig. 1). This is particularly relevant because the major neural pathways controlling lower urinary tract function emerge in humans at these levels [9].
The etiology of enuresis remains a topic of debate; however, this study demonstrated an association between spina bifida occulta with dysplastic development of the sacral vertebral arches and pediatric enuresis. This may lead to occult neural dysfunction at the sacral spinal cord level, impairing the control of lower urinary tract function. Spina bifida is a congenital birth defect that occurs when the spinal bone and spinal cord do not form properly; this is classified as a type of neural tube defect. However, spina bifida occulta, the mildest form of spinal dysraphism, is rarely included in studies of neural tube defects due to its frequent lack of detection and uncertainty regarding its relationship to overt spina bifida [14]. The incidence of spina bifida occulta in enuretic children has been previously reported to fall between 35% and 70% [3-6]. Currently, it is unclear whether spina bifida occulta at the sacral vertebral level can cause any type of neural abnormalities, either structural or functional, leading to lower urinary tract dysfunction related to nocturnal enuresis. We hypothesize that unfused sacral arches create a gap that may expose autonomic and somatic nerves originating from the sacral level, resulting in nerve stimulation at night. However, further evaluation, including neurological testing, is necessary to elucidate the relationship between enuresis and occult neural damage due to unfused sacral arches.
The reported effectiveness of folic acid in preventing spina bifida is well documented [15-17]. As nocturnal enuresis may be linked to spina bifida occulta at the sacral level, it is possible that taking folate supplements during pregnancy could help prevent this condition. However, further research is necessary to confirm this.
One potential concern regarding the use of 3D-CT to detect dysplastic development of sacral arches in children with enuresis is the amount of radiation exposure, given that nocturnal enuresis is primarily a benign and/or self-limiting condition. However, previous studies have reported a low response rate to treatment in enuretic children with spina bifida occulta [7,8], and the 3D-CT technique may be usable to detect dysplastic changes in the sacrum. The 3D-CT method could be valuable for stratifying individual future care plans for enuretic children who may be resistant to conventional treatment. Further research on the risks versus benefits of 3D-CT is necessary prior to its clinical implementation.
In most children, the sacral vertebral arches at the S1–3 levels fuse by the age of 10. However, our study reveals that children with nocturnal enuresis display a significantly higher prevalence of unfused sacral arches. This finding suggests that dysplastic development of the sacral vertebral arches may contribute to the pathogenesis of nocturnal enuresis. The dysplastic sacral arches observed in patients with nocturnal enuresis appear to resemble those found in spina bifida occulta. Consequently, future research employing pelvic 3D-CT imaging techniques may prove valuable in clarifying the development of preventive or therapeutic approaches for children affected by nocturnal enuresis.
This study had some limitations. First, the functional relationship between enuresis and occult neural damage due to unfused sacral arches was not clarified. Thus, further studies such as neurological testing and voiding function analysis are necessary to clarify this point. Second, this study is still preliminary, with a small sample size for each study group; therefore, our results may not be generalizable to the entire population of enuresis patients. Consequently, future studies investigating the relationship between enuresis and unfused sacral arches will be planned with a larger study population.
NOTES
REFERENCES
1. Nevéus T, von Gontard A, Hoebeke P, Hjälmås K, Bauer S, Bower W. The standerdization of terminology of lower urinary tract function in children and adolescents: report from the Standardization Committee of the International Children’s Continence Society. Society J Urol 2006;176:314-24. PMID: 16753432

2. Arda E, Cakiroglu B, Thomas DT. Primary nocturnal enuresis: a review. Nephrourol Mon 2016;8:e35809. PMID: 27703953



3. Ritchey ML, Sinha A, DiPietro MA, Huang C, Flood H, Bloom DA. Significance of spina bifida occulta in children with diurnal enuresis. J Urol 1994;152:815-8. PMID: 8022022


4. Samuel M, Boddy SA. Is spina bifida occulta associated with lower urinary tract dysfunction in children? J Urol 2004;171:2664-6. PMID: 15118447


5. Miyazato M, Sugaya E, Nishijima S, Oowan T, Ogawa Y. Location of spina bifida occulta and ultrasonographic bladder abnormalities predict the outcome of treatment for primary nocturnal enuresis in children. Int J Urol 2006;14:33-8. 
6. Kumar P, Aneja S, Kumar R, Taluja V. Spina bifida occulta in functional enuresis. Indian J Pediatric 2005;72:223-5. 

7. Shin SH, Im YJ, Lee MJ, Lee YS, Choi EK, Han SW. Spina bifida occulta: not overlooked in children with nocturnal enuresis. Int J Urol 2013;20:831-5. PMID: 23294087


8. Cakiroglu B, Tas T, Eyyupoglu SE, Hazar AI, Balci MBC, Nas Y, et al. The adverse influence of spina bifida occulta on medical treatment outcome of primary monosymptomatic nocturnal enuresis. Arch Italiano Urol e Androl 2014;86:270-3.
9. de Groat WC, Griffiths D, Yoshimura N. Neural control of the lower urinary tract. Compr Physiol 2015;5:327-96. PMID: 25589273


10. Calhoun PS, Kuszyk BS, Heath DG, Carley JC, Fishman EK. Threedimensional volume rendering of spiral CT data. theory and method. Radiographics 1999;19:745-64. PMID: 10336201


11. Nevéus T, Fonceca E, Franco I, Kawauchi A, Kovacevic L, Nieuwhof-Leppink A. Management and treatment of nocturnal enuresis-an updated standardization document from International Children’s Continence Society. J Pediatr Urol 2020;16:10-9. PMID: 32278657

12. Järvelin MR, Vikeväinen-Tervonen L, Moilanen NP, Huttunen NP. Enuresis in seven-year-old children. Acta Pediatr Scand 1988;77:148-53. 
13. Forsythe WI, Redmond A. Enuresis and spontaneous cure rate: Study of 1129 enuretics. Arch Dis Child 1974;49:259-63. PMID: 4830115



14. Botto LD, Moore CA, Khoury MJ, Erickson JD. Neural-tube defects. N Engl J Med 1999;341:1509-19. PMID: 10559453


15. Shurtleff DB. Epidemiology of neural tube defects and folic acid. Cerebrospinal Fluid Research 2004;1:5-8. PMID: 15679939


16. Kondo A, Kamihira O, Ozawa H. Neural tube defects: prevalence, etiology and prevention. Int J Urol 2009;16:49-57. PMID: 19120526


17. MRC vitamin study research group. Prevention of neural tube defects: results of medical research council vitamin study. Lancet 1991;338:131-7. PMID: 1677062

Fig. 1.
Comparison of plain x-ray imaging and 3-dimensional computed tomography (3D-CT) in a 9-year-old boy with enuresis. (A) Using plain x-ray imaging, evaluating the fusion of sacral arches is challenging. (B) 3D-CT clearly displays unfused S1–3 sacral arches, making it an appropriate method for evaluating these structures.
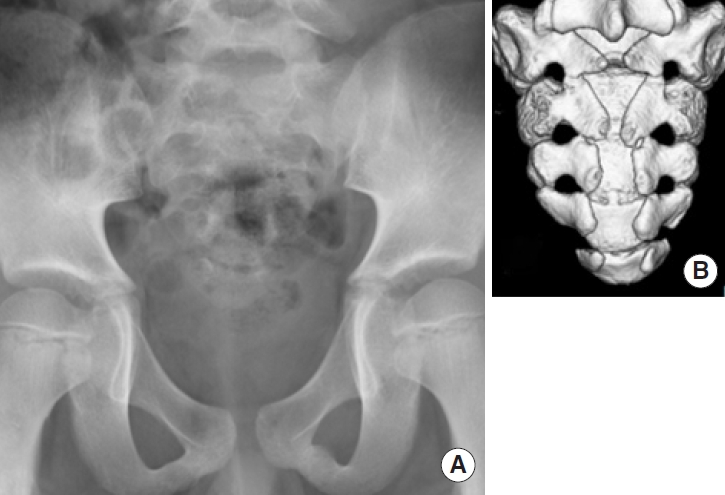
Fig. 2.
Comparison of cases between the enuresis and control groups. (A) Unfused S1–3 arches in an 11-year-old boy with enuresis. (B) Fused sacral arches in an 11-year-old boy without enuresis.
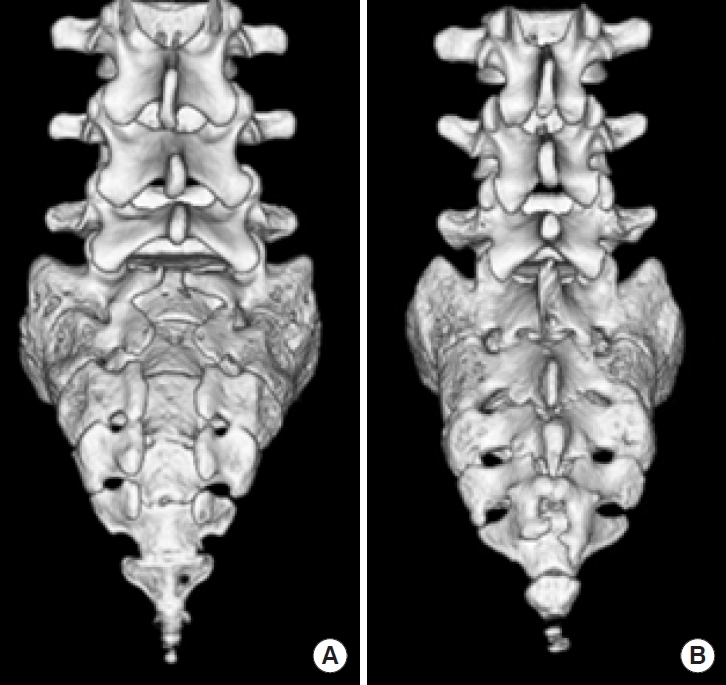
Table 1.
Sacral arch fusion in control and enuresis groups





