|
 |


- Search
| Int Neurourol J > Volume 26(4); 2022 > Article |
|
ABSTRACT
Purpose
The purpose of this study was to investigate the prevalence and risk factors of overactive bladder (OAB) in young adults and to explore the influence of OAB on mental health.
Methods
Between October 2019 and January 2020, 14,010 anonymous questionnaires were distributed to freshmen at 2 universities in Henan, China. The students came from all over the country. The questionnaire included general items and information necessary to calculate the overactive bladder symptom score, the Chinese version of the Pittsburgh Sleep Quality Index (PSQI) score, Self-Esteem Scale (SES) score, and Self-Rating Depression Scale (SDS) score. The relationships between the prevalence of OAB and its risk factors were evaluated.
Results
The overall prevalence of OAB was 6.0%, with 4.3% of participants characterized as having dry OAB and 1.7% as having wet OAB. The prevalence of mild OAB was 5.5%, and that of moderate OAB was 0.5%; no severe OAB was observed. Higher prevalence rates of OAB were found among women, respondents with constipation, and respondents with primary nocturnal enuresis (PNE) (P <0.05). Compared to healthy controls, the OAB group exhibited a higher mean SDS score (52.12±8.986 vs. 47.71±9.399, P<0.001) and mean PSQI score (5.28±2.486 vs. 4.27±2.431, P<0.001), but a lower mean SES score (27.78±3.599 vs. 29.57±4.109, P<0.001).
Overactive bladder (OAB) is a common urological abnormality that is defined by the International Continence Society (ICS) as “urgency, with or without urge incontinence, usually with frequency and nocturia” in the absence of “proven infection or other obvious pathology” [1]. The literature on OAB among young adults is limited, and the results are inconsistent [2-4]. In the United States, the prevalence of OAB with urinary incontinence in those aged 18 to 24 years was reported to be 2.0% among women and 0.3% among men [2]. The prevalence of OAB among Iranian women aged 15 to 29 years was 10.9% [3], while it was only 0.8% among 18- to 29-year-olds in China [4]. In another study in Fuzhou, China, the prevalence of OAB among women aged 20 to 29 years was 5.7% [5]. Therefore, a survey of OAB prevalence in mainland China according to the current ICS definition is necessary.
The etiology and risk factors of OAB have not been fully clarified, although age, sex and body mass index (BMI) are reported risk factors for OAB [4-6]. Additionally, some studies have shown that constipation is closely related to the development of OAB in adults and children [5,7]. Alcohol intake and carbonated beverage intake are also significantly associated with OAB [8]. However, the risk factors for OAB in young adults have not been fully clarified. OAB is well known to impact physiology, psychology, and society [9]. Therefore, understanding the prevalence of OAB, its risk factors, and related urinary symptoms can help define treatment resources and develop preventive
measures in the future.
The purpose of this study was to investigate the prevalence and risk factors of OAB among university students in mainland China. Since university students are a key group of young adults, this study provides important information for further understanding the epidemiology of OAB in young adults in mainland China.
Between October 2019 and January 2020, a survey of 14,010 junior university students was administered at two universities medical university in China using an anonymous questionnaire after obtaining informed consent. The participants originated from areas throughout the country, and they were instructed to avoid taking medication or consuming coffee in the 3 days prior to participation. In addition, all participants underwent a physical examination, including a routine urine examination. The inclusion criteria of the OAB group were as follows: (1) fulfillment of the diagnostic criteria for primary OAB, which include symptoms of urgency, frequent urination, and nocturia, with or without urgent urinary incontinence; and (2) an urgency score of ≥2 and a total score of ≥3 on the overactive bladder symptom score (OABSS). The exclusion criteria were a congenital history of urinary tract abnormality, pelvic surgery, neurogenic disease, or present urinary tract infection (UTI). The presence of UTI was assessed via urine testing, which is part of the routine physical examination conducted at the time of entry to the university. The study was performed according to the Declaration of Helsinki and approved by the Ethics Committee of Xinxiang Medical University (XYLL-2018237).
The contents of the questionnaire included: (1) basic information (such as sex, date of birth, place of origin, height, and weight); (2) history of primary nocturnal enuresis (PNE; intermittent incontinence while asleep in a child >5 years of age, at least twice a month [10]), recurrent UTI, and constipation; (3) urinary frequency, urgency, incontinence and nocturia (used to calculate the OAB symptom score); and (4) scores on the Chinese version of the Pittsburgh Sleep Quality Index (PSQI), Self-Esteem Scale (SES), and Self-Rating Depression Scale (SDS). We explained the urinary tract-related medical terms on the front page of the questionnaire and informed the participants that the survey was anonymous and for research purposes only.
The PSQI was developed to evaluate subjective sleep disturbance over the prior month, with a higher score indicating poorer sleep quality. The Chinese version of the PSQI was translated and validated by Zhu et al. [11] in a sample of college students and patients with insomnia or psychiatric disease. In that study, the internal consistency (Cronbach α) was 0.84. The Chinese version of the SDS has been verified to be applicable to the Chinese population and has been widely used in China [12]. The psychometric properties of the Chinese version of the SES have been empirically tested, and its internal consistency was indicated by an α coefficient of 0.77 [13].
The diagnostic criteria for OAB used in this study were an urgency score of at least 2 and a total OABSS score of at least 3. Dry OAB was defined as OAB without urgent urinary incontinence (as indicated by an urgent urinary incontinence OABSS score of 0), while wet OAB referred to OAB with urgent urgency incontinence (as indicated by an urgent urinary incontinence OABSS score of at least 1). A total OABSS score of 5 or lower was considered to indicate mild OAB, a score between 6 and 11 indicated moderate OAB, and a score of 12 or higher indicated severe OAB.
After verification by the research group staff, the data were imported into the IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA) for statistical analysis. Count data were expressed as percentages, and measurement data were expressed as means±standard deviations. The chi-square test was used to analyze the factors related to OAB, and logistic regression was used for the multivariate analysis. The U-test was used to compare the SDS, SES, and PSQI scores between the OAB and nonOAB groups. A P-value of <0.05 indicated a statistically significant difference. The Bonferroni method was used to correct the test standard (P/α), and comparisons were performed among age groups and BMI groups.
The data for 93.4% (13,083 of 14,010) of the participants (4,192 males and 8,891 females; age, 19±1.3 years) were included in the final statistical analysis.
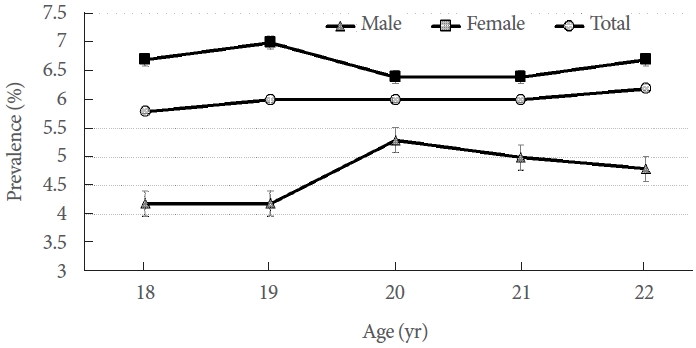
The overall prevalence of OAB was 6.0% (788 of 13,083), with dry OAB accounting for 4.3% (562 of 13,083) and wet OAB accounting for 1.7% (226 of 13,083) of cases. The prevalence of mild OAB was 5.5% (726 of 13,083), and that of moderate OAB was 0.5% (62 of 13,083); no severe OAB was observed. The prevalence rates of OAB among male and female participants were 4.7% (196 of 4,192) and 6.7% (592 of 8,891), respectively, and the difference was significant. The prevalence of OAB was 5.8% (101 of 1,739) among 18-year-olds, 6.0% (227 of 3,766) among 19-year-olds, 6.0% (188 of 3,108) among 20-year-olds, 6.0% (130 of 2,164) among 21-year-olds, and 6.2% (142 of 2,306) among the 22-year-old participants. No correlation was observed between prevalence rate and age (χ2=0.224, P>0.05) (Fig. 1).
The prevalence of OAB with respect to sex, constipation, and PNE is shown in Table 1. A significant relationship was found between OAB prevalence and each of those parameters (P<0.05). No significant relationship was found between OAB prevalence and place of residence, BMI, or age (P>0.05).
The variables found to be meaningful in the chi-square analysis were included in the regression analysis model, and the results showed that female sex (odds ratio [OR], 1.374; 95% confidence interval [CI], 1.159–1.630), constipation (OR, 1.460; 95% CI, 1.236–1.724), and PNE (OR, 2.490, 95% CI, 1.530–4.053) were risk factors for OAB occurrence (Table 2).
Based on the U-test, the SES score of the OAB group was lower than that of the healthy group, while the SDS and PSQI scores were higher than those of the healthy group, as shown in Table 3.
OAB severely affects quality of life due to frequent toilet use, forced reduction of water consumption, and fear of participating in social activities [9]. Many studies have been published on OAB, but none have included specific analysis of the prevalence of OAB in young adults [2,4,5]. Our study can help supplement the data on OAB in young adults in China. This study did not include young adults of all ages; however, since 90% of Chinese young adults attend high school and 80% of senior high school students attend college, the group we chose should be representative of Chinese young adults. In addition, this study was focused on university students, who have a relatively high education level and may be able to better cooperate with the anonymous survey, increasing the reliability of this instrument.
The prevalence of OAB in our study differed from the results of other studies [2,6], which may be due to differences in OAB definitions, study populations, and survey methods (telephone or on-site survey). In our study, the participants were surveyed in person using an anonymous questionnaire based on the standard ICS definition [1]. The National Overactive Bladder Evaluation program defined OAB as the perception of an urgent need to urinate at least 4 times in the past 4 weeks and either urinating at least 8 times a day or using at least 1 coping method [2]. In a study based on the European Prospective Investigation into Cancer and Nutrition (EPIC) program, the prevalence of OAB in those aged ≥18 years was 11.8%; notably, this was the first study to use the 2002 ICS definition to investigate the prevalence of OAB, which was diagnosed based only on the symptoms of urgency incontinence [6]. The above 2 surveys were implemented by telephone, and the response rates were lower than that of our survey. Differences in survey methods may have impacted the results. Moreover, the prevalence rate in our study was lower than those found in other countries, which may be due to cultural and lifestyle-based variations. Caffeine consumption and alcohol intake are well known to be significantly higher among Western populations than in mainland China, and caffeine and alcohol are mild diuretics that can excite detrusors and easily induce detrusor overactivity [8,14,15]. However, whether the consumption of caffeine or alcohol contributes to the observed OAB prevalence remains a matter of debate and should be further investigated in the future [14,15]. To exclude the effects of caffeine or alcohol on the prevalence of OAB, all participants in our study avoided consuming caffeine or alcohol in the 3 days prior to participation.
A study by Wang et al. [4] of 2,425 people aged 18 to 29 years yielded a lower prevalence rate than the present study. A potential reason for this differential finding is that the participants that we surveyed were college students with a high level of education and a strong understanding of medical vocabulary, and they completed the questionnaire more accurately than the respondents in other studies. Moreover, the age range of the participants was larger in the Wang et al. study than in our study, and the number of participants in the former aged 18–22 years is unknown. In addition, the male-to-female ratio of the 2,425 participants in the Wang et al. study was 1:1, and both the sample size and male-to-female ratio were lower than in our study. This may explain the different prevalence rates. Irwin et al. [6] showed that before the age of 60 years, the prevalence of OAB was higher among women than men. However, our study and that of Wang et al. were conducted in mainland China; thus, further research on the prevalence of OAB in young adults is still needed.
Zhang et al. [5] reported prevalence rates of 1.8% for dry OAB and 3.9% for wet OAB among women aged 20 to 29 years, whereas the prevalence of wet OAB among female participants in the present study was lower (1.4%). This discrepancy may be due to the different survey methods and age groups of the participants in the 2 studies. In the study of Zhang et al. [5], the Bristol Female Lower Urinary Tract Symptoms questionnaire was used, and the survey was conducted using email; in contrast, the current study involved use of the OABSS questionnaire to conduct a face-to-face survey of the participants. In the OABSS questionnaire, the wet OAB score for urgent urinary incontinence is at least 1 [16]. The OABSS has been demonstrated to be a practical tool in Chinese clinical studies [4]. Additionally, face-to-face investigations can be used to obtain participant information more accurately than non-face-to-face methods. Furthermore, the age range of the participants in this study was smaller than that in the study of Zhang et al. [5], which may also explain why the prevalence rate of wet OAB was lower.
Many studies have not presented a classification of the severity of OAB [2,4,5]. We classified OAB as mild, moderate, or severe using the OABSS questionnaire and showed that most OAB cases were mild; moderate and severe OAB cases were uncommon. This aligns with the actual situation. However, even mild OAB has a notable effect on young adults. A report from China confirmed that OAB meaningfully affects the quality of life of people over 18 years old [4]. Therefore, young adults with OAB also need timely treatment or intervention.
The prevalence of OAB may vary by sex. The EPIC study indicated that the prevalence of OAB was slightly higher among women than among men [6]. The present study supports this view. This finding may relate to sex-specific anatomical differences, such as the shorter urinary tract in women increasing susceptibility to UTIs. This finding suggests that women should pay particular attention to their urinary tract health in daily life.
The relationship between OAB and BMI has long been controversial. Many studies of adults have indicated that a high BMI is related to a higher likelihood of developing OAB [2,4,7]. Another study reported that OAB was associated with BMI in female university students [17]. The present survey indicated that OAB was not related to BMI, although respondents with BMI ≥30 kg/m2 had an increased tendency to exhibit OAB (Table 1). However, the number of participants with BMI ≥30 kg/m2 was too small to reach definitive conclusions. Additional studies are required to confirm whether BMI is related to OAB in young adults. In addition, we found that living environment was not related to the prevalence of OAB, which was consistent with the conclusions of the Korean research team of Jo et al. [18] The reason for this finding may be that with economic development, the living conditions in urban and rural areas have become similar; therefore, the difference in the impact of urban and rural environments on OAB prevalence has become minimal. A study by Xing et al. [19] reported that the prevalence of OAB among children aged 5 to 14 years was 9.01% and decreased with age. In the present study, the prevalence of OAB was generally stable. Neither this study nor the study by Xing et al. mentioned the prevalence among the 14- to 18-year-old population; therefore, understanding the differences between the 2 studies requires further examination. In the present study, OAB prevalence was not significantly associated with age, which contradicts the view that the prevalence of OAB in adults increases with age, as shown by most researchers [2,4,5]. Additionally, this result could be explained by the small age difference in this study population, meaning that all participants effectively belonged to the same age group.
Research has shown that constipation is a risk factor for OAB [7,20], and our study supports this view. Constipation has been postulated to suppress the common nerves of the bladder and intestine, which leads to a lack of central nerve inhibition of bladder activity, resulting in bladder overactivity [21]. Constipation as a risk factor for OAB is not fully understood. We speculate that it may relate to excessive rectal dilatation and detrusor activity caused by feces remaining in the rectum for a long period of time. Constipation treatment has also been suggested to be necessary during OAB treatment. In the present survey, we found that young adults with PNE were more likely to suffer from OAB than respondents without PNE. A separate study showed that PNE is related to OAB in children [22]. Research has indicated that one-third of patients with OAB have PNE, which may be due to involuntary detrusor activity in patients with PNE [23].
The incidence of acute cystitis is known to increase in young women after the age of 19 to 20 years, and cystitis may be a cause of OAB in adolescents. Unfortunately, this was not considered in our survey due to the difficulty of confirming acute cystitis in this large investigation. Consequently, we excluded individuals with acute UTI, some of whom may have had acute cystitis [24]. The association of cystitis with OAB should be investigated in the future.
The results of this study support the view that OAB has negative effects on psychology, such as reducing sleep quality and increasing the incidence of depression and self-abasement [25]. OAB affects mental health, which may be related to the regulation of bladder function by numerous neural pathways [25]. To avoid compromising the privacy of the participants, we did not collect information on other factors that may affect the students’ psychology, such as economic conditions, violence, and divorce; therefore, the relationship between OAB and psychological disorders requires further study.
In the present study, many risk factors were found for the prevalence of OAB among young adults, with no clear mechanisms. Therefore, researchers must continue to investigate the potential mechanisms behind these relationships. Although the participants originated from around the country, this was not a cross-sectional study, and the information obtained from the survey on the prevalence and risk factors of OAB among young adults may not represent the complete situation of OAB among young adults in China. This survey required respondents to recall and list the symptoms of the disease, which may have promoted recall bias. Additionally, the continuous presence of OAB in an individual over time must be documented. Thus, in this study, we reported only the sensation of urgency in a young sample population and additionally did not evaluate sexual function in the population with OAB. Therefore, multicenter surveys and additional samples are necessary to clarify the potential risk factors and underlying mechanisms of OAB.
In conclusion, OAB is common among Chinese university students and affects their mental health significantly. Female sex, constipation, and PNE were risk factors for OAB.
NOTES
Funding/Grant Support
Henan Province Medical Science Provincial-ministerial Construction Project (No: SBGJ2018059); National Nature Science Foundation of China (No. U1904208).
Research Ethics
The study was performed according to the Declaration of Helsinki and approved by the Ethics Committee of Xinxiang Medical University (XYLL-2018237).
AUTHOR CONTRIBUTION STATEMENT
·Conceptualization: YL, JGW, CPS
·Data curation: YL, GWS, HJH, JGW, ZZ, QFD
·Formal analysis: YL, GWS, HJH, ZZ, QFD
·Funding acquisition: JGW
·Methodology: YL, ZZ, CPS
·Project administration: YL, GWS, HJH, JG Wen, ZZ, CPS, QFD
·Visualization: YL, HJH, ZZ, CPS, QFD
·Writing - original draft: YL
·Writing - review & editing: YL, GWS, HJH, JGW, CPS
REFERENCES
1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 2002;21:167-78. PMID: 11857671


2. Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol 2003;20:327-36. PMID: 12811491



3. Safarinejad MR. Prevalence of the overactive bladder among Iranian women based on the International Continence Society definition: a population-based study. Int Urol Nephrol 2009;41:35-45. PMID: 18563617



4. Wang Y, Xu K, Hu H, Zhang X, Wang X, Na Y, et al. Prevalence, risk factors, and impact on health related quality of life of overactive bladder in China. Neurourol Urodyn 2011;30:1448-55. PMID: 21826714



5. Zhang W, Song Y, He X, Huang H, Xu B, Song J. Prevalence and risk factors of overactive bladder syndrome in Fuzhou Chinese women. Neurourol Urodyn 2006;25:717-21. PMID: 16944449


6. Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 2006;50:1306-14 discussion 1314-5. PMID: 17049716


7. Kim SY, Bang W, Choi HG. Analysis of the prevalence of and factors associated with overactive bladder in adult Korean women. PLoS One 2017;12:e0185592. PMID: 28957446



8. Robinson D, Hanna-Mitchell A, Rantell A, Thiagamoorthy G, Cardozo L. Are we justified in suggesting change to caffeine, alcohol, and carbonated drink intake in lower urinary tract disease? Report from the ICI-RS 2015. Neurourol Urodyn 2017;36:876-81. PMID: 28444711



9. Rapariz M, Mora AM, Roset M. Impact of overactive bladder symptoms on work activity: the ACTIVHA study. Actas Urol Esp (Engl Ed) 2018;42:176-84. PMID: 29103735


10. Nørgaard JP, van Gool JD, Hjälmås K, Djurhuus JC, Hellström AL. Standardization and definitions in lower urinary tract dysfunction in children. International Children’s Continence Society. Br J Urol 1998;81 Suppl 3:1-16. PMID: 9634012

11. Zhu B, Xie M, Park CG, Kapella MC. Adaptation of the Pittsburgh Sleep Quality Index in Chinese adults with type 2 diabetes. J Chin Med Assoc 2018;81:242-7. PMID: 29258729



12. Li H, Lei J, Xu F, Yan C, Guimerans M, Xing H, et al. A study of sociocultural factors on depression in Chinese infertile women from Hunan Province. J Psychosom Obstet Gynaecol 2017;38:12-20. PMID: 27934537


13. Xue-Yan Z, Dong-Mei L, Dan-Dan X, Le-Shan Z. Obese Chinese primary-school students and low self-esteem: a cross-sectional study. Iran J Pediatr 2016;26:e3777. PMID: 27713806



14. Schimpf MO, Smith AR, Miller JM. Fluids affecting bladder urgency and lower urinary symptoms (FABULUS): methods and protocol for a randomized controlled trial. Int Urogynecol J 2020;31:1033-40. PMID: 31875256



15. Miller JM, Schimpf MO, Hawthorne K, Hortsch SB, Garcia C, Smith AR. Fluids affecting bladder urgency and lower urinary symptoms: results from a randomized controlled trial. Int Urogynecol J 2022;33:1329-45. PMID: 35435467



16. Yamaguchi O, Nishizawa O, Takeda M, Yokoyama O, Homma Y, Kakizaki H, et al. Clinical guidelines for overactive bladder. Int J Urol 2009;16:126-42. PMID: 19228224


17. Hagovska M, Švihra J, Buková A, Horbacz A, Dračková D, Švihrová V. Comparison of body composition and overactive bladder symptoms in overweight female university students. Eur J Obstet Gynecol Reprod Biol 2019;237:18-22. PMID: 31003045


18. Jo JK, Lee S, Kim YT, Choi HY, Kim SA, Choi BY, et al. Analysis of the risk factors for overactive bladder on the basis of a survey in the community. Korean J Urol 2012;53:541-6. PMID: 22949998



19. Xing D, Wang YH, Wen YB, Li Q, Feng JJ, Wu JW, et al. Prevalence and risk factors of overactive bladder in Chinese children: a population-based study. Neurourol Urodyn 2020;39:688-94. PMID: 31804751



20. Cornu JN, Amarenco G, Bruyere F, Chartier-Kastler E, Fatton B, Grise P, et al. Prévalence et prise en charge initiale de l’hyperactivité vésicale en France : une étude transversale. Prog Urol 2016;26:415-24 French. PMID: 27108102


21. Aguiar LM, Franco I. Bladder bowel dysfunction. Urol Clin North Am 2018;45:633-40. PMID: 30316317


22. Sousa AS, Veiga ML, Braga AA, Carvalho MC, Barroso U Jr. Enuresis and overactive bladder in children: what is the relationship between these two conditions? Int Braz J Urol 2016;42:798-802. PMID: 27564293



23. Suditu N, Negru I, Miron A, Novac B, Ciuta C. Is nocturnal enuresis a predisposing factor for the overactive bladder? Turk J Med Sci 2019;49:703-9. PMID: 31203588



24. Dobberfuhl AD. Pathophysiology, assessment, and treatment of overactive bladder symptoms in patients with interstitial cystitis/ bladder pain syndrome. Neurourol Urodyn 2022;41:1958-66. PMID: 35607890



25. Felde G, Ebbesen MH, Hunskaar S. Anxiety and depression associated with urinary incontinence. A 10-year follow-up study from the Norwegian HUNT study (EPINCONT). Neurourol Urodyn 2017;36:322-8. PMID: 26584597



Table 1.
Univariate analysis of the prevalence of and risk factors for OAB among 13,083 university students
Table 2.
Logistic regression analysis of the influencing factors of OAB prevalence
| Variable | β | SE | P-value | OR (95% CI) |
|---|---|---|---|---|
| Sex | 0.318 | 0.087 | < 0.001 | 1.374 (1.159–1.630) |
| Constipation | 0.379 | 0.085 | < 0.001 | 1.460 (1.236–1.724) |
| PNE | 0.912 | 0.249 | < 0.001 | 2.490 (1.530–4.053) |