 |
 |


- Search
| Int Neurourol J > Volume 26(2); 2022 > Article |
|
ABSTRACT
Methods
Data were obtained from the National Health and Nutrition Examination Survey 2005–2010. Mortality data were obtained by linking the primary database to death certificate data found in the National Death Index with mortality follow-up up to December 31, 2015. Nocturia was defined based on symptoms reported in the symptom questionnaire. We categorized patients into 2 groups: mild nocturia (2–3 voids/night) and moderate-to severe nocturia (≥4 voids/night). Multiple Cox regression analyses were performed with adjustment for confounding variables at the baseline survey.
Results
This study included 9,892 adults (4,758 men, 5,134 women). Nocturia occurred in 3,314 individuals (33.5%). Nocturia was significantly associated with all-cause mortality (hazard ratio [HR], 1.23; 95% confidence interval [CI], 1.10–1.39) and cardiovascular disease (CVD) mortality (HR, 1.55; 95% CI, 1.19–2.01). Moreover, the mortality risk increased with increasing nocturia severity. Further analysis with propensity score matching showed that nocturia was still significantly associated with all-cause mortality and CVD mortality. In subgroup analysis according to sex, nocturia was significantly associated with allcause mortality and CVD mortality in men. In women, moderate-to-severe nocturia was significantly associated with allcause mortality and CVD mortality. In subgroup analysis according to cardio-metabolic diseases, nocturia was associated with CVD mortality in patients with diabetes mellitus, hypertension, dyslipidemia, or CVD at baseline. In subgroup analysis of patients without diabetes mellitus, hypertension or CVD, nocturia was significantly associated with all-cause mortality.
Nocturia was defined by the International Continence Society (ICS) in 2002 as a complaint of waking at night for one or more times to void [1], but they updated this definition in to waking at night to pass urine during the main sleep period [2]. Nocturia is a highly prevalent and bothersome lower urinary tract symptom among older adults and the general population [3]. About 30 years ago, the prevalence of nocturia was about 25% in women and 20% in men [4], but recently, with an increase in the older population, this prevalence has increased to 34.9% in women and 30.5% in men [5]. Although, some reports have suggested that the prevalence reaches 60% in men and women over 70 years old [6,7].
Nocturia has been associated with many comorbidities including cardiovascular diseases (CVDs) (such as coronary heart disease, hypertension, and heart failure), and endocrine disorders (such as diabetes mellitus and central diabetes insipidus) [4,5,8]. It has also been associated with chronic illnesses, such as chronic respiratory disease, neurological disease, and malignancy [9]. Considering its associations with these many chronic comorbid conditions, several studies have reported a relationship between nocturia and mortality [3,4,9]. However, despite the increase in nocturia and comorbidities in older people, this relationship cannot be completely explained in terms of older age, and related evidence in the literature is limited. To optimally assess the effect of nocturia on mortality while minimizing the risk of bias, fluctuations in nocturia and follow-up after the initial evaluation should be considered, and a validated nocturia assessment and reliable registration of all deaths during follow-up should be used [9].
The National Health and Nutrition Examination Survey (NHANES), a nationally representative population-based sample of the United States, was conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention [5]. To date, only a few studies have investigated nocturia [10] or its association with mortality [4] using NHANES data. Only one study reported an association between nocturia and mortality risk using NHANES III 1988–1994, but the data used is about 30 years old [4]. Therefore, we investigated the relationship between nocturia and mortality risk in the United States using the NHANES data collected between 2005 and 2010.
The NHANES is a biannual national representative survey to evaluate the health and nutritional status of populations in the United States. It is a cross-sectional study that samples participants who undergo health and nutrition questionnaire-based surveys, physical examinations, and laboratory tests. The National Center for Health Statistics’ Research Ethics Review Board approved the NHANES protocol (Protocol #2005-06), and each participant provided written consent. Household surveys included demographic and socioeconomic data as well as health and nutritional status information. Anthropometric measures and laboratory tests were conducted using standardized protocols. We obtained baseline data, including nocturia questionnaire information, anthropometric data, and laboratory data using 3 cycles of NHANES from 2005 to 2010. We linked the mortality information to baseline data from NHANES 2005 to 2010. The mortality information of NHANES was obtained from public-use linked mortality files at the National Center for Health Statistics, which was based on the probabilistic match between NHANES and National Death Index death certificate records up to December 31, 2015 [11].
Nocturia was defined based on the symptom questionnaire. We categorized the participants into 2 groups based on the frequency of nocturia into mild (2–3 voids/night) and moderateto-severe (≥4 voids/night) according to the classification criteria used in previous studies [12,13]. Covariates in this analysis included age, sex, race/ethnicity, smoking status, alcohol consumption, body mass index (BMI), sleep duration, and metabolic disorders at baseline survey such as dyslipidemia, hypertension, diabetes mellitus, and CVD. Hypertension was defined as follows: average value of 3 recorded systolic blood pressures >140 mmHg, average diastolic blood pressure >90 mmHg, or hypertension treatment. Diabetes mellitus was defined as follows: fasting blood glucose >126 mg/dL, random blood glucose >200 mg/dL, hemoglobin A1c >6.5%, or diabetes mellitus treatment. We defined dyslipidemia as fasting total cholesterol >240 mg/dL or dyslipidemia treatment.
Continuous variables are presented as means±SD with P-values according to nocturia using the t-test. Categorical variables are presented as numbers (%) with P-values using the chisquare test. We estimated hazard ratios (HRs) using multiple Cox proportional hazard regression analyses to investigate the effect of nocturia on all-cause mortality and CVD mortality. Moreover, considering the heterogeneity of the confounding variables according to nocturia, we conducted subgroup analysis with propensity score matching data (1:1 matching) using R version 3.1.0 (The R Foundation for Statistical Computing, Vienna, Austria). A P-value of <0.05 was considered statistically significant. Statistical analysis was performed using IBM SPSS Statistics ver. 24.0 (IBM Co., Armonk, NY, USA).
The study included 9,892 adults (4,758 men, 5,134 women) (Fig. 1). Nocturia occurred in 3,314 individuals (33.5% of total; 31.7% of men; 35.1% of women). The participants’ clinical characteristics obtained from NHANES 2005–2010 are presented in Table 1. Nocturia was more common in older individuals, women, smokers, and those with higher BMI and metabolic diseases. In addition, the prevalence of CVD was significantly higher in those with nocturia at the baseline survey. In the follow-up data up to 2015, adults with nocturia showed a significantly higher incidence of all-cause and CVD mortality than those without nocturia (Table 1).
Kaplan-Meier survival curves revealed a significantly higher rate of all-cause mortality and CVD mortality in participants with nocturia than in those without nocturia (Fig. 2) In the multiple Cox regression analysis, nocturia was significantly associated with all-cause mortality (HR, 1.23; 95% CI, 1.10–1.39; P<0.001) and CVD mortality (HR, 1.55; 95% CI, 1.19–2.01; P =0.001). Mild and moderate-to-severe nocturia were both significantly associated with all-cause mortality (HR, 1.17; 95% CI, 1.03–1.32; P=0.014; HR, 1.67, 95% CI, 1.36–2.06; P<0.001, respectively) and CVD mortality (HR, 1.49; 95% CI, 1.14–1.96; P=0.004; HR, 1.90; 95% CI, 1.20–2.99; P=0.006, respectively) (Table 2). Considering the heterogeneity of the participants with nocturia, additional analysis was performed using 1:1 propensity score matching. With propensity score matching, nocturia was still significantly associated with all-cause mortality (HR, 1.25; 95% CI, 1.10–1.41; P<0.001) and CVD mortality (HR, 1.58; 95% CI, 1.2–2.07; P=0.001). Mild and moderate-tosevere nocturia were significantly associated with all-cause mortality (HR, 1.18; 95% CI, 1.04–1.34; P =0.012; HR, 1.69; 95% CI, 1.37–2.09; P<0.001, respectively) and CVD mortality (HR, 1.52; 95% CI, 1.15–2.02; P =0.004; HR, 1.94; 95% CI, 1.23–3.08; P=0.005, respectively) (Table 2).
The incidence of all-cause mortality according to age group is summarized in Fig. 3. In all age groups, patients with nocturia had a higher incidence of all-cause deaths than those without nocturia. In participants aged ≥61 years, patients with nocturia showed a higher incidence of CVD related deaths than participants without nocturia (7.0% vs. 3.9%, P<0.001). In participants aged 20–60 years, the incidence of CVD related deaths was 1% in patient with nocturia and 0.4% in participants without nocturia (P=0.008). In the multiple Cox regression analysis with subgroup according to age group, nocturia was significantly associated with all-cause mortality in participants aged from 20–60 years (HR, 1.44; 95% CI, 1.08–1.92; P=0.012) and in participants aged ≥61 years (HR, 1.18; 95% CI, 1.04–1.34; P=0.012) (Table 3). Nocturia was significantly associated with CVD mortality in participants aged over 61 years (HR, 1.48; 95% CI, 1.12–1.96; P=0.006). In participants aged 20–60 years, moderate-to-severe nocturia was significantly associated with CVD mortality (HR, 5.59; 95% CI, 2.07–15.08; P=0.001).
Patients with nocturia had a higher incidence of all-cause death and CVD related death than those without nocturia for both sexes (Fig. 3). In the multiple Cox regression analysis for men, nocturia was significantly associated with all-cause mortality (HR, 1.28; 95% CI, 1.09–1.50; P=0.002) and CVD mortality (HR, 1.68; 95% CI, 1.20–2.35; P =0.002) (Table 3). The subgroup analysis in women showed that moderate-to-severe nocturia was significantly associated with all-cause mortality (HR, 1.91; 95% CI, 1.39–2.63; P<0.001) and CVD mortality (HR, 2.82; 95% CI, 1.41–5.01; P=0.003).
Considering the differences in the prevalence of cardio-metabolic diseases at baseline according nocturia, subgroup analysis stratified by risk factors for all-cause mortality and CVD mortality was conducted (Table 4). Nocturia was associated with CVD mortality in patients with cardio-metabolic diseases including diabetes mellitus, hypertension, dyslipidemia or CVD at baseline. In those without diabetes mellitus, hypertension or CVD at baseline, nocturia was significantly associated with allcause mortality.
Our study using data from NHANES 2005–2010 reported that 33.5% of participants (men, 31.7%; women, 35.1%) had nocturia ( ≥2 voids/night). This was an increase from a previous study reporting on NHANES III (1988–1994), which showed that the prevalence of nocturia (≥2 voids/night) was 15.5% in men and 20.9% in women [4]. This increase may be due to the rapidly aging population. A study of NHANES 2005–2016 reported that more than 80% of those ≥60 years old experienced nocturia ≥1 void/night, while approximately 50% of these experienced nocturia ≥2 voids/night [10]. This is important as the elderly population of the United States will be 88.5 million (20% of the total population) by 2050 [14].
The ICS defines nocturia as voiding that occurs during the main sleep period [2]. However, some physicians do not consider 1 void during sleep hours to be clinically significant. This may be because some studies have reported that <2 voids/night is not bothersome and that ≥2 voids/night can compromise the quality of life [15,16]. In this study, we defined nocturia as ≥2 voids during sleep at night. We also categorized mild nocturia as 2–3 voids during sleep at night and moderate-to-severe nocturia as ≥4 voids during sleep at night. Based on this definition and categorization, we showed that nocturia is a dose-dependent predictor of mortality, where mortality risk increased as the episodes of nocturia increased. The results of the present study are consistent with those reported in previous studies [3,4,9,17].
Our results are also consistent with previous reports from a United States population-based study. In NHANES III 1988– 1994, nocturia ( ≥2 voids/night) was associated with poorer survival compared with 0–1 void in men and women [4]. This association was particularly notable in subjects below 65 years old, with attenuated associations in those ≥65 years old. The current study also analyzed survival according to age group. Nocturia (≥2 voids/night) was associated with poorer survival and this association was particularly notable in participants aged 20–60 years, with attenuated associations in participants aged ≥61 years old.
Two recent studies [3,9] investigated the association between nocturia and mortality, and a systematic review and meta-analysis of 11 observational studies has revealed an association between nocturia and mortality [9]. In this analysis, nocturia was defined as 2 or 3 voids on separate occasions and was associated with increased mortality (risk ratio, 1.27; 95% CI, 1.16–1.40) [9]. In a longitudinal, 5-year, general population cohort study of 9,762 Japanese men and women, subjects with nocturia were at greater risk of death than those without nocturia in a dose-dependent manner (HR 1.46 for 1 time, 95% CI, 1.02–2.09; HR 1.85 for 2 times, 95% CI, 1.23–2.77; and HR 2.06 for ≥3 times, 95% CI, 1.28–3.32) [3].
Multiple pathways are considered to underlie the relationship between nocturia and mortality [3]. Sleep loss can negatively affect health by decreasing immune function and increasing the risk of CVD, obesity, and type 2 diabetes mellitus [5,18]. These comorbidities could lead to death, suggesting that chronic illnesses are associated with nocturia and mortality. More specifically, sleep disturbance due to nocturia could increase CVD mortality by inhibiting physiological nighttime blood pressure drop and increasing sympathetic activity [19]. Moreover, fractures and other injuries resulting from falls associated with severe nocturia and daytime fatigue could impair performance status and cause frailty, which could lead to death [9,20]. Thus, nocturia has been associated with falls and fractures, in addition to an increased risk of chronic illnesses (such as CVD, hypertension, and diabetes) [4].
In the present study, there was a significantly higher prevalence of CVD events at baseline and CVD mortality in those with nocturia. Particularly, compared with all-cause mortality, CVD mortality showed a higher HR. Our results indicate that nocturia severity was associated with an increased risk of all-cause mortality (HR, mild vs. moderate-severe nocturia, 1.14 vs. 1.62 before, and 1.18 vs. 1.69 after propensity score matching). Interestingly, the dose-dependent relationships were even more prominent in CVD mortality (HR, mild vs. moderate-severe nocturia, 1.43 vs. 1.58 before, and 1.52 vs. 1.94 after propensity score matching). Therefore, our findings indicate that the risk of CVD and all-cause mortality increased as the episodes of nocturia increased.
In a previous report of 70-year-old adults, subjects with nocturia had a greater risk of CVD than those without nocturia (HR, 2.16; 95% CI, 1.01–4.61) suggesting that nocturia is a predictor of mortality in older patients with CVD [17]. Several studies have shown that CVD is associated with nocturia in both clinical and community-based populations [4,17,21,22]. In the Boston Area Community Health study, CVD was independently correlated with nocturia (odds ratio [OR], 1.37; 95% CI, 1.01–1.87), [22] and in the Finnish National Nocturia and Overactive Bladder study, CVD was associated with nocturia in women (OR 3.13; 95% CI, 1.48–6.64) [21].
In our subanalysis, nocturia in men and women without CVD at the baseline survey was associated with the risk of allcause mortality. However, nocturia was associated with the risk of CVD mortality only in men, regardless of the presence of CVD at baseline. These results suggest that nocturia is a risk factor for all-cause mortality in men and women when the effect on CVD is excluded. However, CVD mortality was associated with nocturia in men, suggesting sex differences in CVD [23].
This study had several potential limitations. First, participants did not complete a frequency volume chart (FVC). To minimize the risk of bias in analyses of the association between nocturia and mortality, FVC and the self-reported questionnaire are necessary. However, FVC is difficult to apply in the population representative large scale NHANES data set. Researchers emphasize that fluctuations in nocturia should be considered to minimize the risk of bias [9]. On the other hand, Vaughan et al. [24] reported that there was no significant increase in the prevalence of nocturia and the overall regression and progression were balanced in a post hoc analysis of the United States Department of Veterans Affairs Cooperative Studies Program Benign Prostatic Hyperplasia Study. Second, we excluded many participants due to missing data and conducted our research as a cross-sectional study, resulting in limited power. Several studies have found a relationship between nocturia and hip fractures in older people, and nocturia among these older populations is likely to cause hip fractures and death [25,26]. However, we did not have data to determine the association between nocturia and the risk of hip fractures and subsequent mortality risk in this population. Therefore, prospective studies are needed to identify the causal relationship between nocturia and mortality.
The main strengths of our study were the use of a nationally representative large population-based sample of men and women and the high response rate, which enables us to accurately determine the association between nocturia and mortality. Another strength of our study was that all-cause mortality and CVD mortality were analyzed separately, and the investigation of mortality risk according to the severity of nocturia was conducted. Thus, it was possible to investigate in detail whether the cause of death was CVD and if the positive association between nocturia and mortality risk increased with increased nocturia severity. Finally, through full data and 1:1 propensity score matching analysis for confounding variables, a more accurate analysis could be made regarding the causal relationship between nocturia and mortality.
In conclusion, our population-based study demonstrated that mortality was significantly associated with mild and moderateto-severe nocturia in men and women after adjusting for major confounding factors. Our study also showed that CVD mortality was associated with nocturia in a dose-dependent manner. To our knowledge, this study is one of the most recent and largest investigations of the relationship between nocturia and mortality using a nationally representative population-based cohort. Our study provides strong support for the previously established relationship between nocturia and mortality. Moreover, our results should help clarify the mechanisms of nocturia and the relationship between nocturia and mortality risk.
NOTES
REFERENCES
1. van Kerrebroeck P, Abrams P, Chaikin D, Donovan J, Fonda D, Jackson S, et al. The standardisation of terminology in nocturia: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 2002;21:179-83. PMID: 11857672


2. Hashim H, Blanker MH, Drake MJ, Djurhuus JC, Meijlink J, Morris V, et al. International Continence Society (ICS) report on the terminology for nocturia and nocturnal lower urinary tract function. Neurourol Urodyn 2019;38:499-508. PMID: 30644584



3. Funada S, Tabara Y, Setoh K, Negoro H, Akamatsu S, Yoshino T, et al. Impact of nocturia on mortality: the nagahama study. J Urol 2020;204:996-1002. PMID: 32396408


4. Kupelian V, Fitzgerald MP, Kaplan SA, Norgaard JP, Chiu GR, Rosen RC. Association of nocturia and mortality: results from the Third National Health and Nutrition Examination Survey. J Urol 2011;185:571-7. PMID: 21168875


5. Moon S, Chung HS, Yu JM, Ko KJ, Choi DK, Kwon O, et al. The association between obesity and the nocturia in the U.S. population. Int Neurourol J 2019;23:169-76. PMID: 31260617




6. Bosch JL, Weiss JP. The prevalence and causes of nocturia. J Urol 2013;189:S86-92. PMID: 23234639


7. Lombardo R, Tubaro A, Burkhard F. Nocturia: the complex role of the heart, kidneys, and bladder. Eur Urol Focus 2020;6:534-6. PMID: 31395515


8. Bliwise DL, Howard LE, Moreira DM, Andriole GL, Hopp ML, Freedland SJ. Nocturia and associated mortality: observational data from the REDUCE trial. Prostate Cancer Prostatic Dis 2019;22:77-83. PMID: 30214036



9. Pesonen JS, Cartwright R, Vernooij RWM, Aoki Y, Agarwal A, Mangera A, et al. The impact of nocturia on mortality: a systematic review and meta-analysis. J Urol 2020;203:486-95. PMID: 31364920


10. Soysal P, Cao C, Xu T, Yang L, Isik AT, Turan Kazancioglu R, et al. Trends and prevalence of nocturia among US adults, 2005-2016. Int Urol Nephrol 2020;52:805-13. PMID: 31858342



11. Centers for Disease Control and Prevention; National Center for Health Statistics; Office of Analysis and Epidemiology. The linkage of national center for health statistics survey data to the national death index—2015 linked mortality file (LMF): methodology overview and analytic considerations. Hyattsville (MD): Centers for Disease Control and Prevention; 2019.
12. Moon S, Yu SH, Chung HS, Kim YJ, Yu JM, Kim SJ, et al. Association of nocturia and cardiovascular disease: data from the National Health and Nutrition Examination Survey. Neurourol Urodyn 2021;40:1569-75. PMID: 34036656



13. Akerla J, Pesonen JS, Poyhonen A, Hakkinen J, Koskimaki J, Huhtala H, et al. Impact of lower urinary tract symptoms on mortality: a 21-year follow-up among middle-aged and elderly Finnish men. Prostate Cancer Prostatic Dis 2019;22:317-23. PMID: 30410016



14. Vincent GK, Velkoff VA. The next four decades: The older population in the United States: 2010 to 2050. Suitland (MD): United States Census Bureau; 2010.
15. Tikkinen KA, Johnson TM 2nd, Tammela TL, Sintonen H, Haukka J, Huhtala H, et al. Nocturia frequency, bother, and quality of life: how often is too often? A population-based study in Finland. Eur Urol 2010;57:488-96. PMID: 19361907


16. Hakkinen JT, Hakama M, Shiri R, Auvinen A, Tammela TL, Koskimaki J. Incidence of nocturia in 50 to 80-year-old Finnish men. J Urol 2006;176:2541-5 discussion 5. PMID: 17085153


17. Bursztyn M, Jacob J, Stessman J. Usefulness of nocturia as a mortality risk factor for coronary heart disease among persons born in 1920 or 1921. Am J Cardiol 2006;98:1311-5. PMID: 17134620


18. Knutson KL, Ryden AM, Mander BA, Van Cauter E. Role of sleep duration and quality in the risk and severity of type 2 diabetes mellitus. Arch Intern Med 2006;166:1768-74. PMID: 16983057


19. Obayashi K, Saeki K, Kurumatani N. Independent associations between nocturia and nighttime blood pressure/dipping in elderly individuals: the HEIJO-KYO cohort. J Am Geriatr Soc 2015;63:733-8. PMID: 25900486



20. Pesonen JS, Vernooij RWM, Cartwright R, Aoki Y, Agarwal A, Mangera A, et al. The impact of nocturia on falls and fractures: a systematic review and meta-analysis. J Urol 2020;203:674-83. PMID: 31347956


21. Tikkinen KA, Auvinen A, Johnson TM 2nd, Weiss JP, Keranen T, Tiitinen A, et al. A systematic evaluation of factors associated with nocturia--the population-based FINNO study. Am J Epidemiol 2009;170:361-8. PMID: 19515794



22. Fitzgerald MP, Litman HJ, Link CL, McKinlay JB, Investigators BS. The association of nocturia with cardiac disease, diabetes, body mass index, age and diuretic use: results from the BACH survey. J Urol 2007;177:1385-9. PMID: 17382738


23. Lightner DJ, Krambeck AE, Jacobson DJ, McGree ME, Jacobsen SJ, Lieber MM, et al. Nocturia is associated with an increased risk of coronary heart disease and death. BJU Int 2012;110:848-53. PMID: 22233166



24. Vaughan CP, Johnson TM 2nd, Haukka J, Cartwright R, Howard ME, Jones KM, et al. The fluctuation of nocturia in men with lower urinary tract symptoms allocated to placebo during a 12-month randomized, controlled trial. J Urol 2014;191:1040-4. PMID: 24333108


25. Temml C, Ponholzer A, Gutjahr G, Berger I, Marszalek M, Madersbacher S. Nocturia is an age-independent risk factor for hip-fractures in men. Neurourol Urodyn 2009;28:949-52. PMID: 19301408


26. Moon S, Chung HS, Kim YJ, Kim SJ, Kwon O, Lee YG, et al. The impact of urinary incontinence on falls: A systematic review and meta-analysis. PLoS One 2021;16:e0251711. PMID: 34010311



Fig. 1.
Flowchart for participant selection. NHANES, National Health and Nutrition Examination Survey.
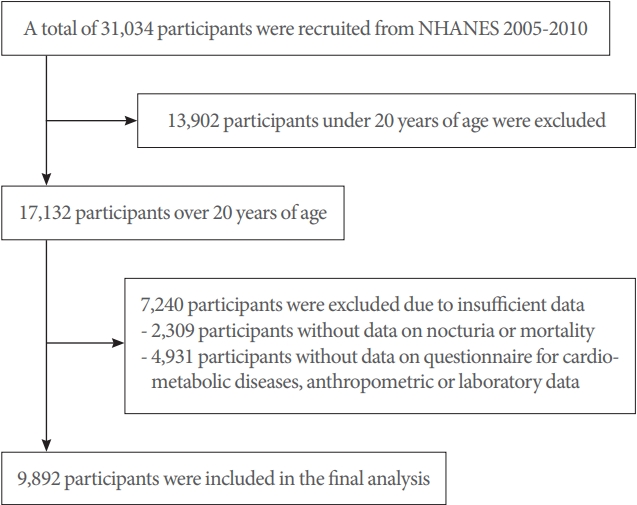
Fig. 2.
Kaplan-Meier curves of mortality according to nocturia. (A) All-cause mortality. (B) Cardiovascular disease mortality.

Fig. 3.
Incidence of deaths according to age and sex. (A) All-cause mortality. (B) Cardiovascular disease mortality.

Table 1.
Participants’ clinical characteristics obtained from the National Health and Nutrition Examination Survey dataset between 2005 and 2010
Table 2.
The association between nocturia and mortality
Table 3.
Association between nocturia (≥2 times) and mortality stratified by age and sex
Table 4.
Association between nocturia (≥2 times) and mortality according to comorbidities
Multiple Cox regression model adjusted for age, race, body mass index, smoking status, alcohol consumption, sleep duration, dyslipidemia, hypertension, and diabetes mellitus.
HR, hazard ratio; CI, confidence interval; DM, diabetes mellitus; HTN, hypertension; DLP, dyslipidemia; CVD, cardiovascular disease.





