Transurethral Procedures for Lower Urinary Tract Symptoms Resulting From Benign Prostatic Enlargement: A Quality and Meta-Analysis
Article information
Abstract
Purpose:
Thanks to advancements in surgical techniques and instruments, many surgical modalities have been developed to replace transurethral resection of the prostate (TURP). However, TURP remains the gold standard for the surgical treatment of benign prostatic hyperplasia (BPH). We conducted a meta-analysis on the efficacy and safety of minimally invasive surgical therapies for BPH compared with TURP.
Methods:
This meta-analysis used a Medline search assessing the period from 1997 to 2011. A total of 784 randomized controlled trials were identified in an electronic search. Among the 784 articles, 36 randomized controlled trials that provided the highest level of evidence (level 1b) were included in the meta-analysis. We also conducted a quality analysis of selected articles.
Results:
Only 2 articles (5.56%) were assessed as having a low risk of bias by use of the Cochrane collaboration risk of bias tool. On the other hand, by use of the Jadad scale, there were 26 high-quality articles (72.22%). Furthermore, 28 articles (77.78%) were assessed as high-quality articles by use of the van Tulder scale. Holmium laser enucleation of the prostate (HoLEP) showed the highest reduction of the International Prostate Symptom Score compared with TURP (P<0.0001). Bipolar TURP, bipolar transurethral vaporization of the prostate, HoLEP, and open prostatectomy showed superior outcome in postvoid residual urine volume and maximum flow rate. The intraoperative complications of the minimally invasive surgeries had no statistically significant inferior outcomes compared with TURP. Also, there were no statistically significant differences in any of the modalities compared with TURP.
Conclusions:
The selection of an appropriate surgical modality for BPH should be assessed by fully understanding each patient’s clinical conditions.
INTRODUCTION
Benign prostatic hyperplasia (BPH), which causes lower urinary tract symptoms (LUTS), is one of the most common diseases of aging men [1]. LUTS can reduce quality of life by impeding normal activities and causing complications such as acute urinary retention or urinary tract infection. BPH is histologically observed in about half of men in their 60s and in most men aged 80 and older [2]. Nowadays, various medications are used to treat LUTS resulting from BPH (LUTS/BPH); these include 5-alpha-reductase inhibitors (5-ARIs), alpha-adrenergic blockers, and others. Moreover, many surgical treatment methods have been introduced, such as resection or enucleation.
Currently, the gold standard surgical treatment for LUTS/BPH is transurethral resection of the prostate (TURP) [3,4]. However, TURP is associated with complications including bleeding, pain, infection, urethral stricture, bladder neck contraction, erectile dysfunction, incontinence, and retrograde ejaculation [5]. Therefore, many endoscopic surgical methods have been suggested to replace TURP as the new standard [6]. There has been a continuous rise in the use of minimally invasive surgical therapies for LUTS/BPH, including bipolar TURP, bipolar transurethral vaporization of the prostate (TUVP), holmium laser enucleation of the prostate (HoLEP), and potassium-titanyl-phosphate (KTP) laser vaporization of the prostate. So far, numerous articles have reported on comparisons of these new techniques with TURP. Ahyai et al. [6] reported a meta-analysis on functional outcomes and complications of transurethral prostatectomy for LUTS/BPH. According to those authors, many minimally invasive surgical therapies for LUTS/BPH showed statistically comparable efficacy and overall morbidity to TURP. However, that report included randomized controlled trials published from 1997 to 2009.
Therefore, we conducted a meta-analysis on the efficacy and safety of minimally invasive surgical therapies for LUTS/BPH compared with TURP by analyzing more recent articles that were published from 2010 to 2011. In addition, we assessed the quality of these articles by using the Jadad scale, the van Tulder scale (VTS), and Cochrane collaboration risk of bias tool (CCRBT).
MATERIALS AND METHODS
Searching Strategy
This meta-analysis used a Medline search assessing the period from 1997 to 2011. We searched published articles by using MeSH phrases such as “benign prostatic hyperplasia,” “enlargement,” and “obstruction”; “minimally invasive surgical therapy”; “randomized controlled trial [Publication Type]”; and the specific TURP name. There were no limitations on languages.
Study Selection
A total of 784 randomized controlled trials were identified in an electronic search. Among the 784 articles, 36 randomized controlled trials that provided the highest level of evidence (level 1b) were included in the meta-analysis. Studies that were not randomized or that had no comparator were excluded.
Data Extraction
We collected the following data: comparator; name of first author; year of publication; number of patients in each group; follow-up period; baseline data, including age, prostate volume (cm3), International Prostate Symptom Score (IPSS), quality of life (QoL) score, postvoiding residual urine volume (PVR; mL), and maximum flow rate (Qmax; mL/sec) before the procedure (Table 1); perioperative outcomes, including operative time (min), weight of resected tissue (g), and length of catheter use (day); functional outcomes, including IPSS and Qmax after the surgery; and complications (Table 2).

Summary of (mean) baseline characteristics from included randomised trials comparing minimally invasive therapies with transurethral resection of the prostate
Quality Analysis
We assessed the quality of the selected articles by using the Jadad scale, VTS, and CCRBT [7]. All quality assessments of articles were performed by two reviewers. If there were different outcomes, the two reviewers and a third reviewer resolved the discrepancy in the results through discussion.
Statistical Analysis
The primary endpoint of the present analysis was functional outcomes, including IPSS/QoL and Qmax/PVR; perioperative results, including operative time (min) and length of catheter use (day); and incidence rate of complications, including bleeding, blood transfusion, conversion to TURP, capsule perforation, transurethral resection syndrome, acute urinary retention, clot retention, secondary apical resection, secondary coagulation revision, secondary bleeding, infection, urethral stricture, bladder neck stenosis, urgency, stress urinary incontinence, and re-operation/intervention requirement. Pooled odds ratios and 95% confidence intervals were calculated for the dichotomous and continuous outcome data between the various operative methods and TURP, respectively. The Q-statistic was used to analyze heterogeneity [8]. If I2 >50%, we considered it as heterogeneous and a random effect model was performed. IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA) and SAS ver. 9.1.3 (SAS Institute, Cary, NC, USA) were used for the statistical analysis. All tests were two-sided, with a significance level of 0.05.
RESULTS
Quality Analysis of Selected Articles
Among the 36 articles, only 2 articles (5.56%) were assessed as having a low risk of bias, 7 articles (19.44%) were assessed as having a moderate risk of bias, and 27 articles (0.75%) were evaluated as having a high risk of bias by use of the CCRBT. On the other hand, by use of the Jadad scale, there were 26 high-quality articles (72.22%). Furthermore, 28 articles (77.78%) were assessed as high-quality articles by use of the VTS.
Meta-Analysis of Functional Outcomes
IPSS (Fig. 1) and QoL (Fig. 2)

Forest plot of International Prostate Symptom Score (IPSS). CI, confidence interval; TURP, transurethral resection of the prostate; IPSS, International Prostate Symptom Score; TUVP, transurethral vaporization of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.

Forest plot of quality of life (QoL, question 8 of the IPSS). CI, confidence interval; TURP, transurethral resection of the prostate; IPSS, International Prostate Symptom Score; TUVP, transurethral vaporization of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
Only KTP laser vaporization of the prostate showed an inferior outcome compared with TURP (P=0.0272). Otherwise, HoLEP showed the highest reduction of the IPSS compared with TURP (P<0.0001). Moreover, only HoLEP showed a higher QoL, although it was not statistically significant (P=0.1252).
Maximum flow rate (Fig. 3) and postvoid residual urine volume (Fig. 4)
Forest plot of maximum flow rate (Qmax). CI, confidence interval; TURP, transurethral resection of the prostate; IPSS, International Prostate Symptom Score; TUVP, transurethral vaporization of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
Forest plot of postvoid residual urine volume (PVR). CI, confidence interval; TURP, transurethral resection of the prostate; IPSS, International Prostate Symptom Score; TUVP, transurethral vaporization of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
Only KTP showed an inferior outcome in Qmax and PVR (P= 0.1407, P =0.0058). However, bipolar TURP, bipolar TUVP, HoLEP, and open prostatectomy showed a superior outcome in Qmax and PVR. Open prostatectomy and HoLEP could not be statistically analyzed for PVR owing to insufficient data.
Meta-Analysis of Complications Of Surgery
Intraoperative complications (Fig. 5)
Forest plot of intraoperative complications. TURP, transurethral resection of the prostate; OR, odds ratio; CI, confidence interval; TUVP, transurethral vaporization of the prostate; Ho-LEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
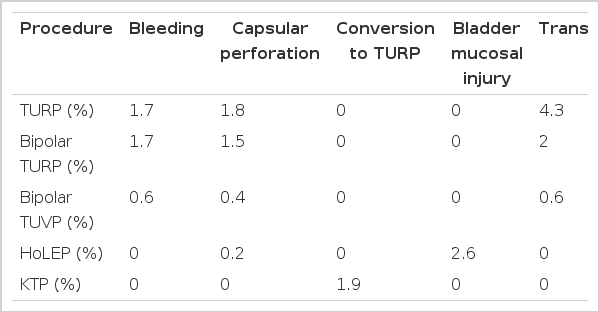
No surgical methods showed statistically significant inferior outcomes compared with TURP. However, HoLEP showed the highest complication rate (P=0.0710) and KTP showed a statistically significantly lower complication rate than TURP (P< 0.0001). HoLEP showed the highest incidence of bladder mucosal injury, and TURP showed the highest incidence of intra-operative transfusion (Table 3).
Perioperative complications (Fig. 6)
Forest plot of perioperative complications. OR, odds ratio; CI, confidence interval; TURP, transurethral resection of the prostate; TUVP, transurethral vaporization of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
KTP and HoLEP showed statistically significantly inferior outcomes compared with TURP (P<0.0001, P=0.0342, respectively). Acute urinary retention, secondary apical resection, and febrile urinary tract infection occurred most commonly with KTP. TURP showed the highest occurrence rate of clot retention and hematuria episodes (Table 4).
Late complications (Fig. 7)
Forest plot of late complications. OR, odds ratio; CI, confidence interval; TURP, transurethral resection of the prostate; TUVP, transurethral vaporization of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
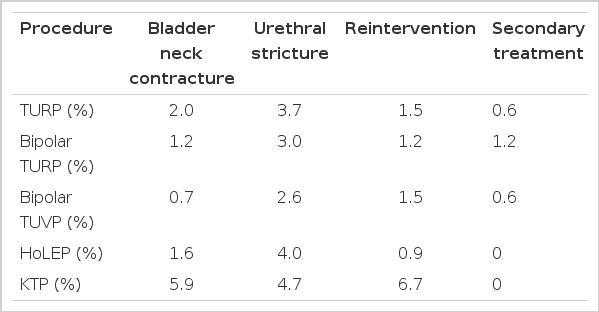
There were no statistically significant differences in any of the modalities compared with TURP. However, bladder neck contracture, urethral stricture, dysuria, and reintervention episode occurred more commonly in the KTP group than in the others (Table 5).
DISCUSSION
BPH results from the proliferation of smooth muscle cells and epithelial cells in the prostatic transitional zone [9]. The treatment of LUTS/BPH is aimed at improving QoL and preventing complications such as urinary tract infection and urinary retention. Treatment methods are largely divided into surgery, medical treatment, and watchful waiting [10]. Watchful waiting is applicable to patients with mild symptoms or with moderate-to-severe symptoms but no complications. This treatment option requires measurement of prostate volume and Qmax annually [11]. For medical management, representative drugs are 5-ARIs and alpha-adrenergic blockers. 5-ARI lowers the serum dihydrotestosterone level and reduces the volume of the prostate [12]. Alpha-adrenergic blockers improve voiding symptoms by relaxation of smooth muscle in the prostate [13]. However, when patients have concomitant complications such as hematuria, infection, or urinary tract obstruction, surgical management is warranted [14]. Many surgical techniques have been developed, such as open prostatectomy, HoLEP, KTP, TURP, bipolar TURP, and bipolar TUVP. Until now, TURP has remained the gold standard treatment option for LUTS/BPH [11]. However, TURP faces many challenges, such as morbidity and functional outcomes [15].
TURP
Accord to our results, TURP was one of the most effective surgical modalities for relieving the obstruction due to BPH. This method needed less reintervention and showed effectiveness for relieving the voiding symptoms, including reduction of IPSS and improvement of Qmax. However, as shown in Tables 3 and 4, TURP has many intraoperative and perioperative complications, such as bleeding, clot retention, and transfusion. Nonetheless, the late complication rate was not inferior compared with other surgical methods. Considering these results, TURP is a worthy mode of surgical intervention for treating LUTS/BPH.
Bipolar TURP
In our meta-analysis, bipolar TURP showed comparable functional outcomes to TURP. Moreover, bipolar TURP showed a shorter length of Foley catheterization and lower intraoperative and perioperative complications. However, to replace TURP, long-term, large-scale, randomized controlled trials will be needed.
HoLEP
Many articles have shown that for large prostates, HoLEP shows superior functional outcomes to open prostatectomy [16,17]. Some parameters of HoLEP, such as length of hospital stay and duration of Foley catheterization, showed supremacy to TURP. Moreover, HoLEP seemed to be effective for avoiding intraoperative and perioperative complications, even though it showed bladder mucosal injury during morcellation of resected prostate adenoma. To confirm the effectiveness and safety of HoLEP, many studies should be performed in relatively small prostates, and long-term comparative studies are needed.
KTP Laser Vaporization of the Prostate
For small to moderate prostate volume, KTP showed comparable functional outcomes, such as for Qmax, PVR, IPSS, and QoL, to TURP. Also, KTP had some benefits, such as a lower incidence of intraoperative complications compared with TURP in patients with a small to moderate prostate volume. However, KTP showed a higher incidence of late complications, such as bladder neck contracture and urethral stricture. Thus, long-term, large-scale randomized controlled studies, conducted for large prostates, should be conducted to prove the usefulness and safety of KTP.
We conducted a meta-analysis of transurethral surgeries for LUTS/BPH. It will be helpful to identify the advantages and disadvantages of each surgical modality. However, we conducted the meta-analysis without a quality analysis of the articles. This is a limitation of the present study even though we performed our analysis of the articles that showed the highest level of evidence.
In conclusion, this study showed statistically comparable efficacy and overall morbidity of transurethral surgeries compared with TURP. Functional outcomes and complications at each step varied for each modality. The selection of an appropriate surgical modality for BPH should be assessed by fully understanding each patient’s clinical conditions.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
SUPPLEMENTARY MATERIALS
Supplementary material can be found via http://www.einj.org/src/sm/inj-17-59-s001.pdf.